Treating Lupus
This site is intended for healthcare professionals as a useful source of information on the diagnosis, treatment and support of patients with lupus and related connective tissue diseases.
The goal and aim of treatment is to reduce the risk of multisystem flares and prevent damage to organs. Lupus is an inflammatory condition that can respond well to different types of drugs. All treatment for lupus is prescribed when the benefits of the drugs outweigh the risks. Medication is chosen dependant on what symptoms are occurring, which organs are affected, and how severe the flare is.
Lupus disease activity, or flare, can be categorised as mild, moderate or severe.
• A mild SLE flare or activity level would include fatigue, malar rash, diffuse alopecia, mouth ulcers, arthralgia, myalgia, &/or platelets 50-149 x10*9/L.
• Moderate disease activity would include fever due to SLE (not linked to infection), lupus-related rash up to 18% body surface area (BSA, this is the standard dermatological unit of measurement), cutaneous vasculitis, alopecia with scalp inflammation, arthritis, pleurisy, pericarditis, hepatitis, &/or platelet count 25-49 x 10*9/L.
• Severe flares include rash involving 18% or more body surface area, myositis, severe pleurisy and/or pericarditis with effusion, ascites, enteritis, myelopathy, psychosis, acute confusion, optic neuritis, platelets <25 x 10*9/L.
Ideally only one long acting immunosuppressant or antimalarial medication should be added or altered at a time, with a sufficient pause before additional alterations to prove what agent is having effect, or to see where side effects are attributable. Steroids may need to be given as well to settle an acute inflammation quickly.
Further detailed information can be found on the British Society of Rheumatology (BSR) web site in the guideline section with specifics for lupus treatment, and nonbiologic DMARD (disease modifying anti-rheumatic drug) monitoring.
• BSR guideline for managing SLE
READ HERE
• BSR guideline for non-biologic DMARD monitoring
READ HERE
Lupus disease activity, or flare, can be categorised as mild, moderate or severe.
• A mild SLE flare or activity level would include fatigue, malar rash, diffuse alopecia, mouth ulcers, arthralgia, myalgia, &/or platelets 50-149 x10*9/L.
• Moderate disease activity would include fever due to SLE (not linked to infection), lupus-related rash up to 18% body surface area (BSA, this is the standard dermatological unit of measurement), cutaneous vasculitis, alopecia with scalp inflammation, arthritis, pleurisy, pericarditis, hepatitis, &/or platelet count 25-49 x 10*9/L.
• Severe flares include rash involving 18% or more body surface area, myositis, severe pleurisy and/or pericarditis with effusion, ascites, enteritis, myelopathy, psychosis, acute confusion, optic neuritis, platelets <25 x 10*9/L.
Ideally only one long acting immunosuppressant or antimalarial medication should be added or altered at a time, with a sufficient pause before additional alterations to prove what agent is having effect, or to see where side effects are attributable. Steroids may need to be given as well to settle an acute inflammation quickly.
Further detailed information can be found on the British Society of Rheumatology (BSR) web site in the guideline section with specifics for lupus treatment, and nonbiologic DMARD (disease modifying anti-rheumatic drug) monitoring.
• BSR guideline for managing SLE
READ HERE
• BSR guideline for non-biologic DMARD monitoring
READ HERE
Analgesia - Analgesia can be prescribed for patients who suffer from joint and muscle pain. NSAIDs (such as ibuprofen both systemic and topical, aspirin or diclofenac) often need to be limited in their use due to side effects, especially in patients with renal problems or high blood pressure.
Anti-malarials -These are especially helpful to patients with skin and joint involvement, to reduce fatigue and can prevent flares and progression to kidney and neurological disease. Unfortunately they take 3-6 months to work, and so patients may require reminding that they need to persevere to gain their benefit. These drugs may be sufficient for patients with mild active lupus to avoid using steroids. Hydroxychloroquine is most commonly used. Mepacrine is sometimes used for skin-only treatment, but can be limited due to the side effects (as it can cause yellowing of the skin). Hydroxychloroquine can cause retinal changes and so in line with recent Royal College of Ophthalmology guidelines, any patient started on this should have baseline ophthalmology screening soon after commencement and follow-up screening annually from 5 years onwards.
Suncreen - At least 4* UVA protection and SPF 50 UVB protection. This familiar skin treatment should not be over looked. It is especially important for patients with proven sun-induced disease and sun-induced rash, however, there is huge value in providing it to all SLE patients with the advice to apply regularly and frequently between April and October and on sunny and/or snowy days over the winter (October to April), even in our sun-poor country. When travelling to hot and sunny countries this application should be increased, with shade seeking, light natural fibre clothing and a broad brimmed hat used to give additional protection.
Suncreen - At least 4* UVA protection and SPF 50 UVB protection. This familiar skin treatment should not be over looked. It is especially important for patients with proven sun-induced disease and sun-induced rash, however, there is huge value in providing it to all SLE patients with the advice to apply regularly and frequently between April and October and on sunny and/or snowy days over the winter (October to April), even in our sun-poor country. When travelling to hot and sunny countries this application should be increased, with shade seeking, light natural fibre clothing and a broad brimmed hat used to give additional protection.
Steroids - Corticosteroids such as prednisolone are powerful anti-inflammatories that can have an immediate effect by controlling active disease in lupus. The dosage depends on the severity of the disease. Once the disease is under control the patient can be weaned off gradually where appropriate, or kept on the lowest dose possible. Although sometimes life-saving, steroids can cause significant side effects especially in those who remain on them at high doses for long periods of time. Important potential side effects of steroid use include infection, osteoporosis, hypertension, cataracts, thin skin and diabetes. Some of these side effects can be lessened dependent on the route of administration and intramuscular (depo-medrone) and intravenous (methyl-prednisolone, MP-IVI) steroids can be beneficial to gain immediate control to patients with significant flaring and with fewer side effects than high dose oral prednisolone.
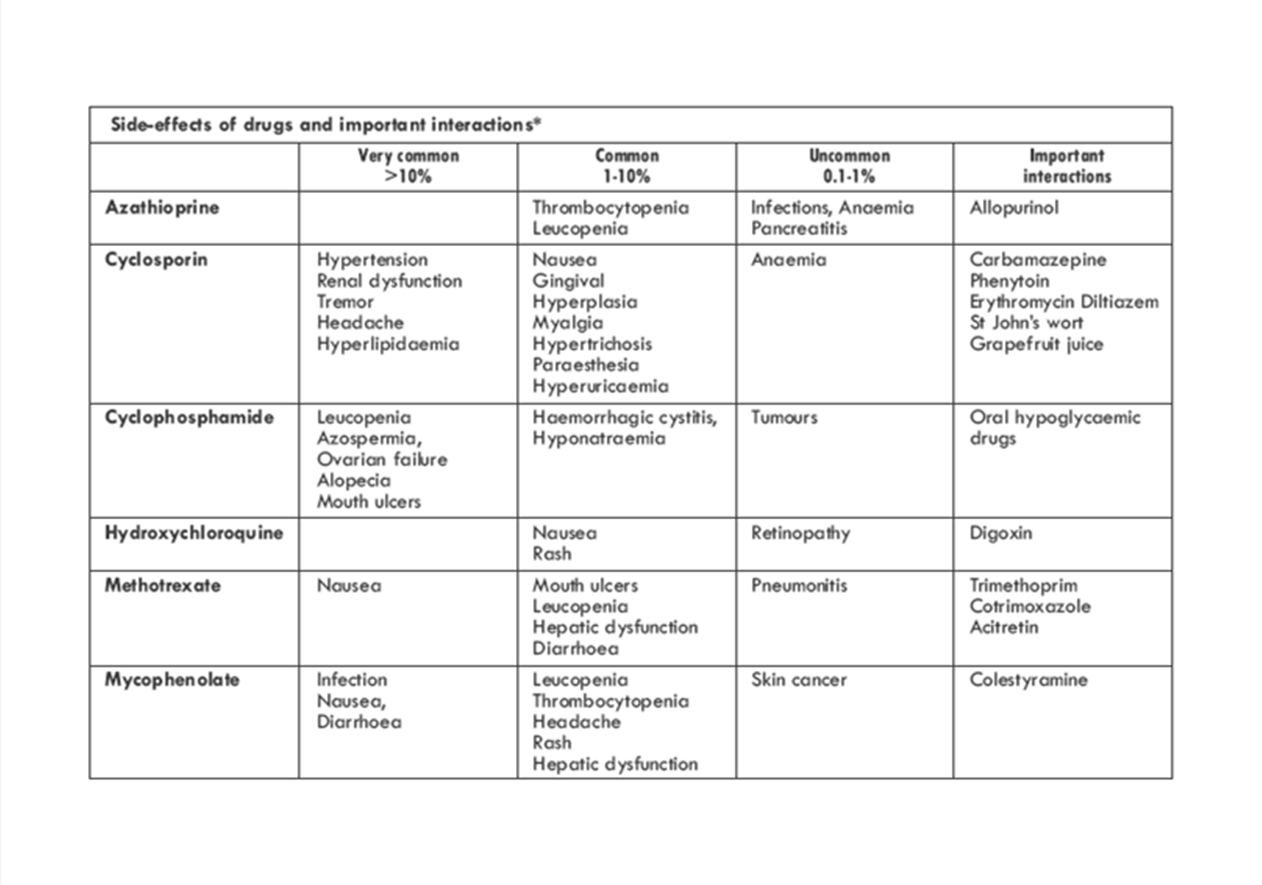
Immunosuppressants - These drugs are widely used in more severe disease. They are very often used to reduce the dose of prednisolone a patient would otherwise need to receive, and so reduce their significant side effect risk. The most commonly used are, methotrexate (always prescribe with supporting folic acid replacement), mycophenolate mofetil, azathioprine (always check TPMT enzyme levels before commencement, which is the intrinsic enzyme needed for drug breakdown and clearance that can be inherently too low), cyclophosphamide, cyclosporine, tacrolimus, & leflunomide. As methotrexate, mycophenolate mofetil, and cyclophosphamide are all teratogenic it is essential all patients both male and female are advised and use sufficiently protective contraception.
Regular blood testing is required at least every two weeks when introducing a new treatment drug and while doses are changing. This should include FBC, creatinine, estimated or calculated GFR (eGFR), ALT &/or AST and albumin levels. As guided by the BSR this needs to be for a minimum of 6 weeks until a stable dose is established. Once stable, blood tests need to be repeated every 4 weeks for 3 months, then at least every 12 weeks whilst on medication as these drugs also suppress the blood forming cells in the bone marrow, and can lead to hepatic dysfunction with some immunosuppressants.
(SOURCE)
Regular blood testing is required at least every two weeks when introducing a new treatment drug and while doses are changing. This should include FBC, creatinine, estimated or calculated GFR (eGFR), ALT &/or AST and albumin levels. As guided by the BSR this needs to be for a minimum of 6 weeks until a stable dose is established. Once stable, blood tests need to be repeated every 4 weeks for 3 months, then at least every 12 weeks whilst on medication as these drugs also suppress the blood forming cells in the bone marrow, and can lead to hepatic dysfunction with some immunosuppressants.
(SOURCE)
SLE treatment strategies for examples of mild, moderate and severe lupus - Table 7. BSR SLE guidelines 2018

Side-effects of drugs and important interactions*
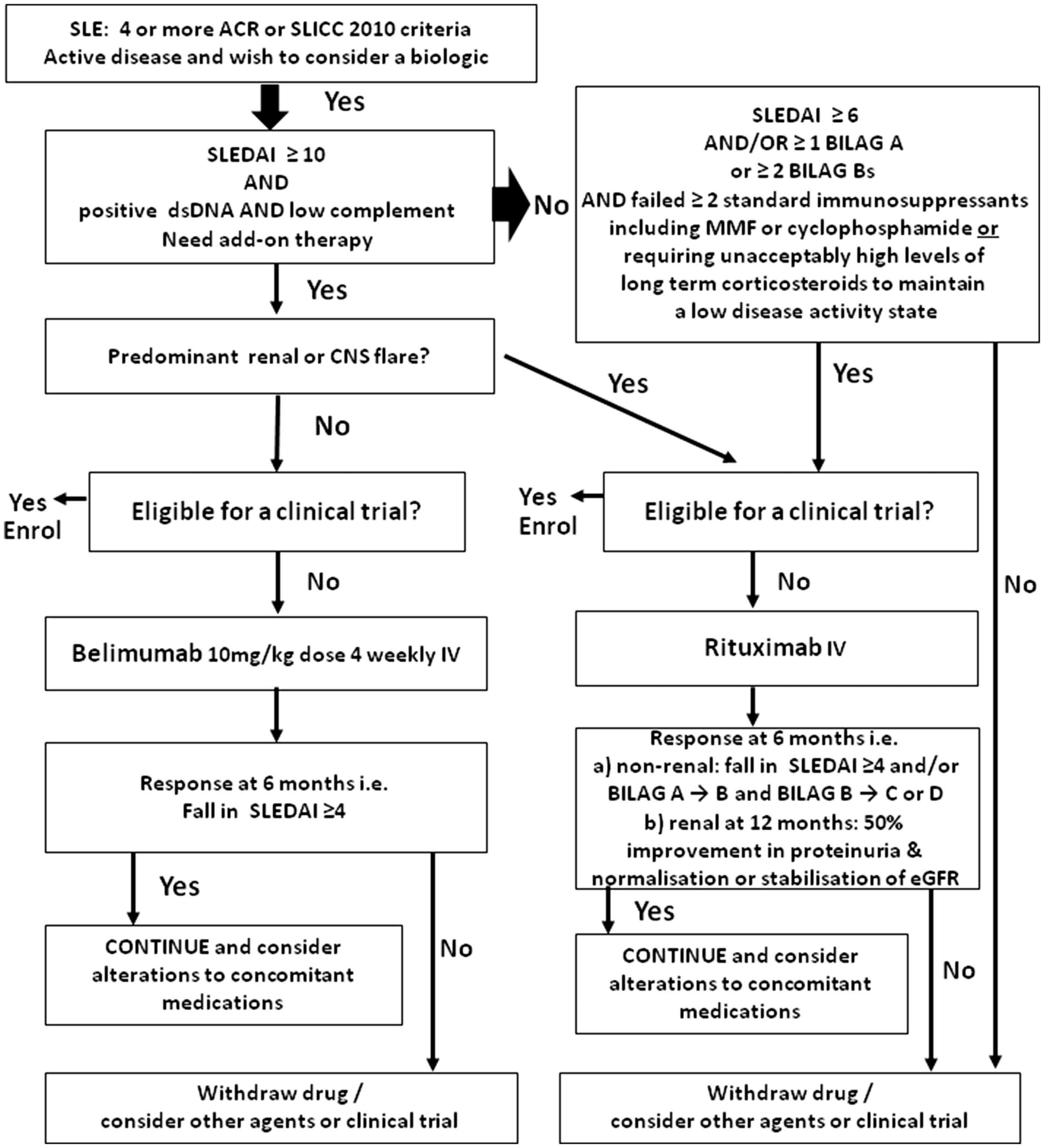
Targeted Monoclonal Antibody Therapies
There are some newer targeted intravenous therapies aimed at B cells which have a pivotal mechanism of action in lupus, which have strict criteria for their use (see figure 1 BSR SLE guideline) SOURCE• Belimumab blocks the activity of a protein called B-lymphocyte stimulator (anti-BLyS), and decreases the amount of circulating abnormal B cells. It is the first drug to have been licensed for SLE since 1955 for those with moderate to highly active lupus. It is given as an IVI treatment initially fortnightly for the first 3 treatments (i.e. weeks 0, 2 & 4), then 4 weekly (i.e. NO treatment week
6, then treatments week 8, 12 etc.). This currently needs to be initiated by a specialist centre, but care can potentially be transferred closer to the patient’s home once established and stable after 6 months of therapy if there is a confirmed response. Since the BSR SLE guidelines were published there
has been a MHRA (Medicines and Healthcare products Regulatory Agency) and UK Government alert (16 Apr 2019) that there is an increased risk of depression, suicidal ideation or behaviour, or self-injury in patients with SLE receiving belimumab compared with those receiving placebo in addition to
standard therapy which should be taken into account before commencing treatment however belimumab remains a suitable treatment for lupus patients with appropriate assessment and care. SOURCE
• Rituximab causes a transient B-cell depletion. This drug binds to the CD-20 molecule on mature B cells and pre-B cells resulting in a decrease in circulating B cells. This gives a more targeted way to switch off a specific portion of the immune system. It is often given as a single course of treatment
of 2 infusions a fortnight apart. Further courses can be given if clinically required, not more frequently than every 6 months.
Other therapies –
o Thalidomide has also been used orally in some cases of aggressive skin disease.
o Prostacyclin analogue (iloprost) or epoprostenol (flolan) infusions may be given for those with Raynaud’s phenomenon where the circulation is severely diminished in the hands and feet.
Drug-induced lupus
It is important to mention there are some drugs that can induce lupus-like symptoms. Although there are many drugs with some link, all SLE patients should avoid those with a proven link, and it is worth bearing in mind for any patient presenting with potential lupus symptoms.
• Minocycline, and other tetracycline antibiotics (most common cause)
• Anti-TNF treatments
• Phenytoin
• Isoniazid
• Chlorpromazine
• Hydralazine
• α-Methldopa
• Procainamide
• Sulphonamides
• Propylthiouracil
Figure 1. BSR SLE guidelines: Summary of NICE and NHS England guidance for the use of belimumab and rituximab in patients with SLE

 ©2024 LUPUS UK (Registered charity no. 1200671)
©2024 LUPUS UK (Registered charity no. 1200671)