
May’s Topic of the Month – Taking Care of Your Nails
 June 01st, 2017
June 01st, 2017 Nakita Cambow
Nakita Cambow Blog
Blog 0 Comments
0 Comments
Fingernail and toenail problems are a common occurrence in people with lupus with many possible abnormalities and potential causes. During medical consultations, these problems may be overlooked as there are often other priorities to discuss. However, it is important to discuss these with your consultant or specialist nurse.
What nail problems can occur in people with lupus?
Quite a few different changes can occur with the fingernails and toenails in people who have lupus. These may be a direct result of having lupus, a side-effect from certain treatments or an indirect consequence of some symptoms. Some of these changes may not necessarily improve with treatment of SLE.
Fungal nail infections
 Fungal nail infections may be more frequent in people with lupus due to some of the medications which can affect the body’s resistance to infection – immunosuppressants. A fungal nail infection may not cause any obvious symptoms at first but as they progress there are a number of potential effects including;
Fungal nail infections may be more frequent in people with lupus due to some of the medications which can affect the body’s resistance to infection – immunosuppressants. A fungal nail infection may not cause any obvious symptoms at first but as they progress there are a number of potential effects including;
- discolouration of the nail – it may turn white, black, yellow or green
- thickening and distortion of the nail – it may become an unusual shape or texture and be difficult to trim
- pain or discomfort – particularly when using or placing pressure on the affected toe or finger
- brittle or crumbly nails – pieces may break off and come away completely
- loose nails
–
“I take daily steroids and have been having problems with fungal infections on finger and toenails. One helpful tip is to seek advice from the pharmacist where you get your repeat medication (they know what drugs you’re on). There are quite a few over-the-counter preparations for it. I found them very helpful! I did have to visit my GP about a fingernail I was worried about and took a sample with me. They tested it at the hospital and confirmed fungal nail and I was prescribed Loceryl ointment which has helped make the nail stronger. They can take a long time to recover and some don’t completely.”
Discoloured nails
The most common causes of a yellow nail are fungal nail infections or nail psoriasis.
Certain medications can cause nails to become discoloured as a side-effect. One of these is mepacrine, an antimalarial that a small percentage of people with lupus may be taking.
Fingernails that are half white and half brown (brown near the tips) can be a sign of kidney failure. It is estimated that this may occur in up to 40% of people with kidney failure. Around 1 in 3 people with SLE develop kidney disease (lupus nephritis) as a symptom. You can learn more about lupus and the kidneys in our booklet HERE.
Other potential causes of nail discolouration include thyroid disease, pregnancy, malnutrition and frequent use of nail varnish.
Loose nails
It is normal for a toenail to come loose and fall off after injury to the toe. This can also occur as a result of over-manicuring the nails and cleaning under them with a sharp object.
Another potential cause for loose nails is poor circulation, such as that caused by Raynaud’s phenomenon. Raynaud’s phenomenon is a common problem that occurs in people who have lupus, appearing in approximately one-third of cases. For tips on coping with this, please visit our blog article HERE.
Indented spoon-shaped nails (koilonychia)
 SLE is one of the conditions which can cause your fingernails to curve inwards like spoons (koilonychia). Other potential causes of this include iron-deficiency anaemia and Raynaud’s phenomenon.
SLE is one of the conditions which can cause your fingernails to curve inwards like spoons (koilonychia). Other potential causes of this include iron-deficiency anaemia and Raynaud’s phenomenon.
Grooves across the fingernails (Beau’s lines)
Deep lines or grooves that go from left to right across the nail are known as Beau’s lines. These can occur due to illness, injury or cold temperatures interrupting nail growth. These could appear following a flare of lupus or exposure to cold temperatures if you have Raynaud’s. The grooves tend to only be noticed a few months later, when the nails have grown and the grooves have moved up the nails to become visible. It takes about four to six months for a fingernail to fully grow out, and six to 12 months for a toenail.
“You get Beau’s lines when you’re not well, so with lupus I am getting quite a few on both thumbs.”
“My nails all have ridges and moons.”
Red or brown little streaks under the nails
 If you have little red or brown streaks underneath your nails, it’s likely they’re splinter haemorrhages – lines of blood caused by tiny damaged blood vessels. A few splinters under one nail are nothing to worry about, and are most likely caused by an injury of the nail. In people with SLE multiple nails may be affected.
If you have little red or brown streaks underneath your nails, it’s likely they’re splinter haemorrhages – lines of blood caused by tiny damaged blood vessels. A few splinters under one nail are nothing to worry about, and are most likely caused by an injury of the nail. In people with SLE multiple nails may be affected.
“I get the splinter-looking lines under my nails. As I have had horses all my life I always assumed they were splinters until I went to Guy’s lupus unit. Since I have been on my medication they had all cleared up until last week when one nail showed signs again. It used to be all of them.”
White nails
A white nail can be the result of the becoming detached from the nail bed, a fungal infection, or a sign of decreased blood supply to the nail bed which can cause something known as “Terry’s Nails”. Terry’s nails are typically white with reddened or dark tips and can be a sign of a wide range of medical conditions. They may be observed in some people who have lupus, such as cases including;
- liver, kidney or heart failure
- diabetes
- iron-deficiency anaemia
- an overactive thyroid
–
Thickened, overgrown nails
In addition to fungal infections, other potential causes of thickened nails are psoriasis or long-term pressure from shoes that are either too small or too narrow over the toes. This may be of concern in those who have swelling in their feet, which will increase the pressure experienced when wearing many shoes.
Nails can also become excessively curved and need to be managed by a podiatrist. Difficulty cutting these curved nails can lead to a spike of nail becoming embedded in the side of the toe (termed as ingrowing toenail). This may become infected with extreme pain being the main symptom with redness and sometimes puss. If you think that you have an ingrowing toe nail or if there is a break in the skin, then medical help is required immediately.
Brittle or crumbly nails
 While this may not be a direct result of lupus, this is something that many people with lupus may experience. Brittle nails are often just a sign of ageing or long-term exposure to water or chemicals such as detergents and nail polish. They can, however, also be the result of an underactive or overactive thyroid (approximately 24% of people with SLE will also develop one of the autoimmune thyroid diseases), or a skin condition called lichen planus.
While this may not be a direct result of lupus, this is something that many people with lupus may experience. Brittle nails are often just a sign of ageing or long-term exposure to water or chemicals such as detergents and nail polish. They can, however, also be the result of an underactive or overactive thyroid (approximately 24% of people with SLE will also develop one of the autoimmune thyroid diseases), or a skin condition called lichen planus.
“My nails constantly break and split to the quick as they are so full of ridges that go down to the nail bed.”
“I have asked about my toenails before and no doctor or rheumatologist knew what was causing them to look horrible. They’re improving slowly now that I’m on an immune suppressant.”
What can I do to look after my nails?
There are a number of things that you can do yourself to take care of your nails and help to keep them healthy. You may wish to try;
 Keeping a good diet. This will help with many things, not just your nails. For tips on diet and healthy eating with lupus, click HERE.
Keeping a good diet. This will help with many things, not just your nails. For tips on diet and healthy eating with lupus, click HERE.- When applying moisturiser to your hands, ensure that you rub some into and around your nails.
- Use an emery board to file nails rather than cutting them (particularly if they are thick or uneven).
- Wear gloves when cleaning or washing.
- Wear comfortable shoes.
- Use as little nail varnish remover as possible, and never use a polish remover containing acetone.
- Avoid biting your nails. This can damage the cuticles, nail bed or potentially risk infection. Anti-nail biting creams or polishes are available, so that when you go to bite your nails it tastes bad. Once you get out of the habit, you can stop using the cream.
- Don’t wear false nails.
- Applying a nail hardener might help strengthen nails.
- Protect yourself against exposure to the cold if you have Raynaud’s.
–
“I have been putting Sally Hanson Strength on my nails. It’s the pink bottle one and it’s been really good at sorting out the ridges and increasing the strength. On top of it I put Sally Hanson Diamond Strength and I no longer get split nails! It’s a breakthrough for me after YEARS of bad nail splitting etc. Any supermarket in the UK has them or Boots etc.”
“I probably shouldn’t, but I have gel overlays on my nails. They are the only thing that stops them breaking/splitting and they cover the ridges.”
“I consume more dairy now; it has been a good source of protein and fat for me. I’ve become allergic to more foods (assuming it’s related to the lupus) but milk, yogurt, and cheese have been fine for me. My nails are in better shape and look healthier.”
“I have my nails done every fortnight (just Gel Polish), but to keep them from breaking I have an IBX treatment. You don’t have to go to a salon; you can purchase it online and apply it yourself. It is an amazing product. I split a nail right down the middle over 20 years ago and have never been able to grow the nail strong again. I have had this treatment and now you can’t even see the split.”
“I’ve started using the Semilac Spa range recently. It’s only been about two weeks using the Spa Muscat for ridges in my nails and I’ve noticed a massive improvement already; my nails look a lot healthier and it also gives a nice milky-white appearance when it’s on.”
“I use Renunail strengthener and nail oil when they feel dry and brittle. Then I do SensatioNail gels at home using the nail shields; they’re great. They are little stick-ons that mean the gel isn’t attached to your actual nail and so you don’t need a damaging soak to remove! I can’t recommend both enough!”
“Perfect Formula from QVC works a treat; it’s the only stuff to have ever made a difference.”
 “Don’t soak them in hot water. Always use rubber gloves for housework.”
“Don’t soak them in hot water. Always use rubber gloves for housework.”
“The only thing to be done, which doesn’t cause further damage, is to moisturise frequently. It helps to sleep with cotton gloves over a very liberal application of moisturising cream.”
“For the ladies saying they file down the ridges; this can cause the nails to be too thin and make them painful over time. When we file them flat we thin the nail to its weakest, thinnest point. I used to do it and over time they got sore and broke really easily. I found a really good ridge-filler base coat years ago, it was only a cheap one but it made my nails smooth and could be used on its own for a natural look or under nail varnish.”
“I frequently moisturise my hands, feet and all my nails in particular. I make sure my vitamin D levels are good. I try to rub pure shea butter into all my cuticles daily.”
To help prevent fungal nail infections you may also wish to;
-
- Keep your nails short, dry, and clean. Stick to one nail clipper for the infected nails and another for the normal ones.
- Don’t just treat your nails; use an antifungal cream to treat any skin that may have athlete’s foot as well.
- Keep your feet dry, wear cotton socks (changed daily), and use ‘breathable’ shoes.
- Normal laundry in hot water should clear any infection from most of the affected socks, but an antifungal spray can be used before laundry for extra effectiveness.
- When you are receiving treatment for fungal infection you don’t need to limit your activities but, to avoid a recurrence, don’t walk barefoot around public pools, showers, and locker rooms.
- Check your feet regularly.
- Avoid cutting the cuticle, either yourself or by a manicurist, since this increases the risk of nail damage and infection.
–
Where can I go for further help with my nails?
Podiatrists
Podiatrists can provide management of infections and problems such as ingrowing toe nails. They can also carry out minor nail surgery.
Podiatrists who work for the NHS are required to register with the Health and Care Professions Council (HCPC) in order to practice. If you see a podiatrist privately, you can check their registration online HERE.
Availability of NHS podiatrists does vary in different areas but people with lupus should be able to have NHS podiatry regardless of age. If you are unsure then ask your consultant or specialist nurse.
 “Every three weeks I have a skilled, experienced manicurist trim and push back my cuticles, and file the ends of my nails; my fingers are too numb to manage this sort of fine self-care. I make sure she doesn’t file the surface of my nails or apply polish because rheumatology and I need to be able to monitor all the diagnostic signs and symptoms my nails, nail beds and nail folds reveal. Every four weeks I see a podiatry nurse who does the same things for my feet. In particular, she especially checks and trims the corners of my big toe nails, which are very prone to becoming ingrown and infected. This is especially important because my forefeet are so numb due to peripheral neuropathy and small cell vasculitis that injury and infection can go unnoticed.”
“Every three weeks I have a skilled, experienced manicurist trim and push back my cuticles, and file the ends of my nails; my fingers are too numb to manage this sort of fine self-care. I make sure she doesn’t file the surface of my nails or apply polish because rheumatology and I need to be able to monitor all the diagnostic signs and symptoms my nails, nail beds and nail folds reveal. Every four weeks I see a podiatry nurse who does the same things for my feet. In particular, she especially checks and trims the corners of my big toe nails, which are very prone to becoming ingrown and infected. This is especially important because my forefeet are so numb due to peripheral neuropathy and small cell vasculitis that injury and infection can go unnoticed.”
Are there any nail treatments I should be cautious of due to my lupus?
Nail manicures and pedicures
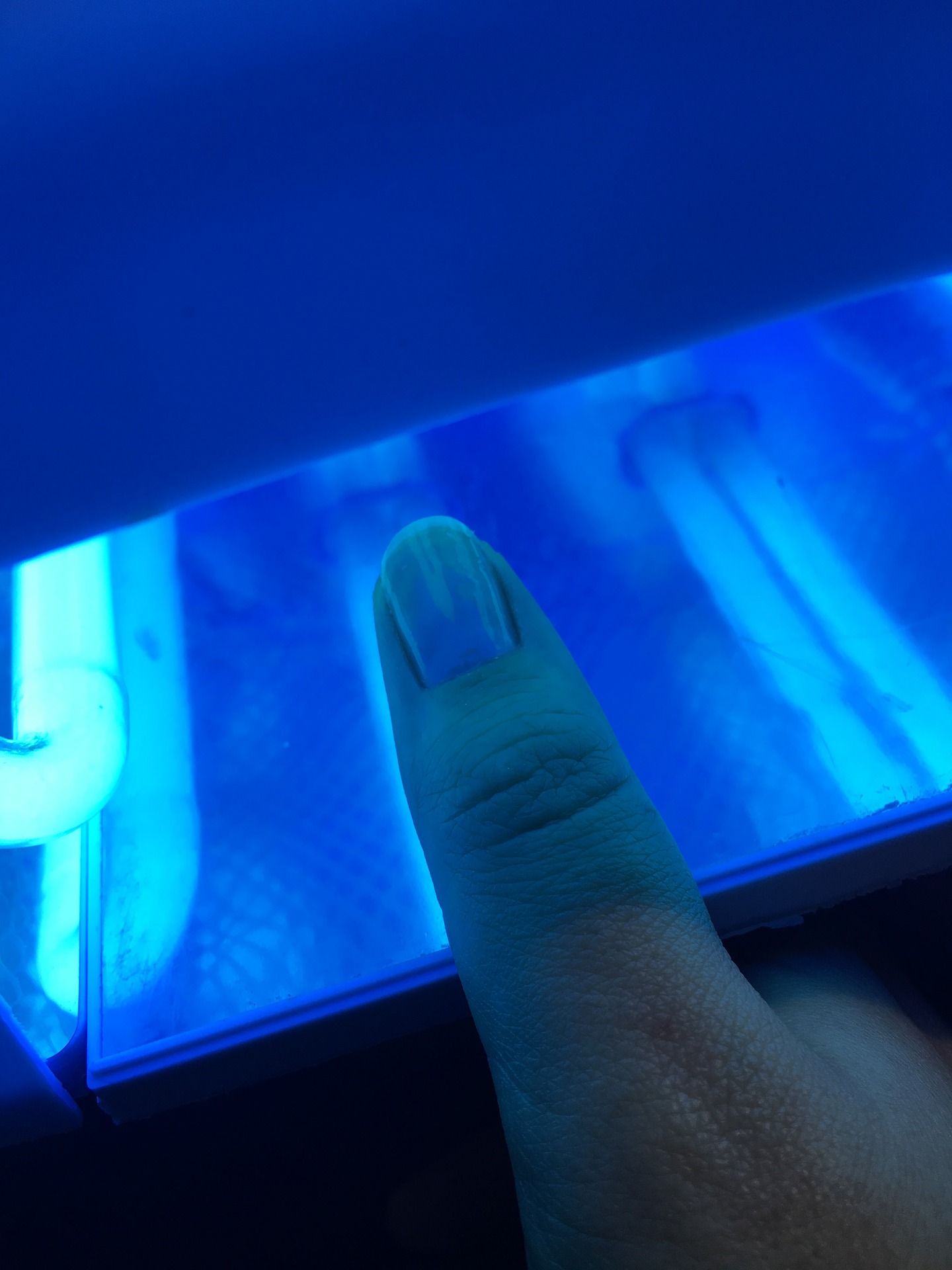 Nail manicures and pedicures are popular, especially the use of gel nails. The lamps used to dry the nails usually emit high levels of UV light and therefore could potentially trigger lupus activity. To play it safe you should avoid manicures or pedicures that require the use of these UV nail drying lamps. Also, be very careful if you enter an establishment that uses them to ensure you are not exposed to them accidentally.
Nail manicures and pedicures are popular, especially the use of gel nails. The lamps used to dry the nails usually emit high levels of UV light and therefore could potentially trigger lupus activity. To play it safe you should avoid manicures or pedicures that require the use of these UV nail drying lamps. Also, be very careful if you enter an establishment that uses them to ensure you are not exposed to them accidentally.
Daniel E. Thomas Jr, quoted a case he came across in ‘The Lupus Encyclopedia’;
“…one of my patients developed a severe flare of her lupus nephritis (kidney inflammation) soon after she started getting gel nails put on her fingers. My very observant nurse fortunately obtained this piece of history for me from the patient.”
Nail varnish containing solvents
 There is some evidence to suggest that exposure to some solvents could trigger lupus to become more active. Trichloroethylene, a commonly used industrial solvent, can have significant effects on the immune system and studies show that it accelerates the onset of lupus in mice. So far, the link between lupus in humans and solvent exposure is weak at best, but to be safe you may wish to avoid any nail varnish that contains trichloroethylene.
There is some evidence to suggest that exposure to some solvents could trigger lupus to become more active. Trichloroethylene, a commonly used industrial solvent, can have significant effects on the immune system and studies show that it accelerates the onset of lupus in mice. So far, the link between lupus in humans and solvent exposure is weak at best, but to be safe you may wish to avoid any nail varnish that contains trichloroethylene.
“I would like to be like the average woman and wear nail varnish, but SLE makes my system over react and when I apply it, the underneath of my nails feel like they are on fire!!! The smell of varnish sets of my asthma too.”
Nail varnish remover
Isopropyl acetone, methyl ethyl ketone, and n-methyl-pyrrolidone, are commonly used as solvents in nail varnish removers. Evidence suggests that these chemicals may cause reproductive harm and organ toxicity. It is therefore important to avoid nail varnish removers containing these chemicals.
“I have learnt not to use nail polish, it doesn’t matter what I use to remove it; it knackers my nails causing them to get very soft and split. If you really want coloured nails used the stick on ones that you can remove before you go to bed.”
Further Reading
NHS Choices – Nail Abnormalities
British Association of Dermatologists – Fungal Infection of the Nails
Campaign for Safe Cosmetics – Products to Avoid
SRUK – What is Raynaud’s?
Thyroid UK
Psoriasis Association
***Please note that this article is written for informational purposes only and should not be a substitute for professional medical advice or treatment. Do not delay seeking or disregard medical advice based on information here. Always seek the advice of your local family physician or other qualified health professional before starting any new treatment or making any changes to existing treatment. It is also advisable to consult a medical professional before making any changes to diet or starting complementary remedies, which may interact with other medications.***
Thank you so much to everyone who submitted their tips and experiences for this month’s topic. We’re sorry if we weren’t able to use your comment in the article this time.




 ©2024 LUPUS UK (Registered charity no. 1200671)
©2024 LUPUS UK (Registered charity no. 1200671)