
July’s Topic of the Month – Caring for your Feet
 August 16th, 2018
August 16th, 2018 Nakita Cambow
Nakita Cambow Blog
Blog 0 Comments
0 Comments
The foot is a complex structure consisting of 26 bones, ligaments, tendons, muscles, blood vessels, nerves, skin and nails. All these work together to influence how we walk and adapt to different activities and the environment.
In the general population, problems associated with these structures are common, but they can have more impact for those people with conditions such as lupus. Generally, lupus does not cause major foot problems but it is good to develop a routine of looking after them. It is important to understand and recognise any changes to the feet and report them to your consultant, specialist nurse or podiatrist. This should result in appropriate treatment and advice in order to prevent any possible deterioration.
Protecting the structure of your feet to prevent/reduce pain
 Inflammation can affect the joints, tendons and ligaments in the feet and/or ankles causing the arch of the foot to reduce in height. An indication that this could be happening is if the heels of your shoes wear out heavily or the upper of the shoe becomes distorted. People may experience pain or aching associated with these changes even if there are no obvious signs of inflammation or swelling.
Inflammation can affect the joints, tendons and ligaments in the feet and/or ankles causing the arch of the foot to reduce in height. An indication that this could be happening is if the heels of your shoes wear out heavily or the upper of the shoe becomes distorted. People may experience pain or aching associated with these changes even if there are no obvious signs of inflammation or swelling.
“On my bad days I have such awful pain in my feet; I can’t put any weight or pressure on them as they are so tender, inflamed, and throbbing around the ball and heel of my foot. Obviously that affects my mobility. I am starting a course of reflexology soon so hopefully that might help.”
As the feet carry the body’s weight and it is not always easy to rest them, these structural changes can become worse over time. This deterioration can potentially be slowed or prevented however if the inflammation is reduced (through medication) and the structures of the feet are supported (with insoles and good footwear).
There are several things that you can do to help protect the structure of your feet;
Choose suitable footwear
 It is important to choose your footwear with comfort, support, and utility in mind. Appropriate shoes will provide support and comfort for the weight-bearing foot with room for the toes to extend fully and to broaden out during weight bearing. Ideally shoes should have a thick, soft cushioned sole, a pliable yielding upper and fasten firmly around the instep, preferably with laces. There should be no high-pressure areas on the feet which rub the skin but plenty of support around the sides of the heel. Seek professional advice in finding shoes suitable for you if necessary.
It is important to choose your footwear with comfort, support, and utility in mind. Appropriate shoes will provide support and comfort for the weight-bearing foot with room for the toes to extend fully and to broaden out during weight bearing. Ideally shoes should have a thick, soft cushioned sole, a pliable yielding upper and fasten firmly around the instep, preferably with laces. There should be no high-pressure areas on the feet which rub the skin but plenty of support around the sides of the heel. Seek professional advice in finding shoes suitable for you if necessary.
Do not wear shoes that cause pain or fatigue. Do not wear women’s high heel shoes or flats. Do not wear sandals or flip flops, or go bare foot. Do not wear shoes tapered or pointed at the toes (i.e., wear shoes with a squared “toe box”). Soft slippers are not helpful as they provide very little support.
“I get really sore feet. Sometimes I wake up with them sore. I always wear Sketchers shoes as they are well cushioned.”
“I wear Birkenstocks which help and I have paid for gait analysis and trainers to suit me which provide massive relief.”
Get supportive insoles
Orthotic inserts can provide needed support and positioning assistance. Consult an experienced professional about the choice of an orthotic, whether having it custom made or obtaining it over the counter.
“I have to have insoles in all of my shoes. If lupus is causing problems ask for a referral to a podiatrist to get proper insoles done for your feet, instead of shop bought. It can make a big difference.”
Plan ahead
 Try to plan appropriate resting time for your feet and avoid excessive walking when your feet are painful. If you work in a job that involves a lot of walking, you may wish to see what support or adjustments may be available to help you manage in your role. You can learn more about this in our employment guides which are available to read and download HERE.
Try to plan appropriate resting time for your feet and avoid excessive walking when your feet are painful. If you work in a job that involves a lot of walking, you may wish to see what support or adjustments may be available to help you manage in your role. You can learn more about this in our employment guides which are available to read and download HERE.
“I try to elevate my feet as much as possible if they are getting swollen and I stretch my legs, feet and ankles. Massaging the soles of your feet before bed is also calming; it is relaxing and eases discomfort.”
“I get intense pain in my feet; I wake up with it. I can’t handle more than four hours at work as the pain is unreal. I always try to hide the fact that I’m in agony. I would hate to be labelled as a complainer.”
Maintain an appropriate weight
 Your feet and ankles carry the weight of your body, so if you are overweight it will add more stress on them. If you need assistance in maintaining a healthy weight you may wish to speak with your GP. For information and advice about lupus and healthy eating, click HERE. For information and advice about lupus and exercise, click HERE.
Your feet and ankles carry the weight of your body, so if you are overweight it will add more stress on them. If you need assistance in maintaining a healthy weight you may wish to speak with your GP. For information and advice about lupus and healthy eating, click HERE. For information and advice about lupus and exercise, click HERE.
Exercises
 If you’re experiencing a muscle or joint problem which is affecting your foot, there are exercises you can try to get you moving normally and safely. NHS Inform has an excellent guide with video demonstrations HERE.
If you’re experiencing a muscle or joint problem which is affecting your foot, there are exercises you can try to get you moving normally and safely. NHS Inform has an excellent guide with video demonstrations HERE.
“A massage with a foot cream is a great relief, albeit only temporary, but I would not be able to sleep without it! They hurt whether I have walked or not, but the worst is the burning sensation!”
Circulation
Three of the conditions below (atherosclerosis, Raynaud’s phenomenon and vasculitis) can reduce the amount of blood reaching the foot and toes and can cause the skin to be thin and dry. The skin may crack (break), ulcerate and then expose the foot to infection. Serious circulatory foot and leg problems are rare but are made worse if the person smokes cigarettes. If you currently smoke and would like to stop, you can get assistance HERE.
If you experience redness, extreme pain and there is a break in the skin, then immediate medical attention is required, as management of an infection requires prompt intervention.
Atherosclerosis
Some people can experience a decreased blood supply to the feet and legs associated with atherosclerosis (hardening of the arteries). This can lead to cramp-like pains in the calf, thigh or buttock muscles whilst walking. To learn more about this condition, including how it is diagnosed and treated, click HERE.
Raynaud’s phenomenon
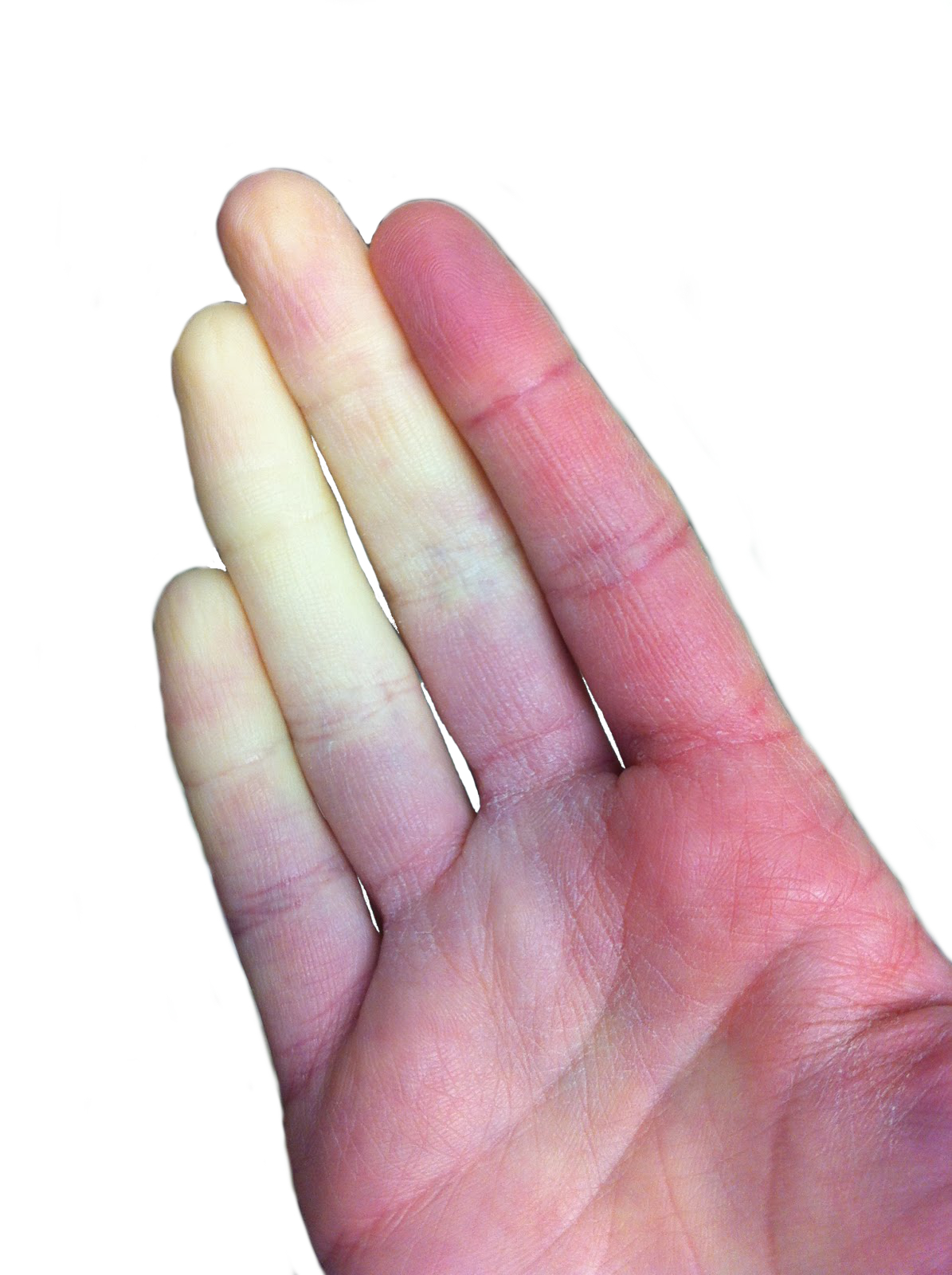 Approximately one-third of people with lupus will experience Raynaud’s phenomenon. In people who have Raynaud’s, the small blood vessels in the extremities are over-sensitive to changes in temperature. This causes a Raynaud’s attack where the toes/feet sometimes change colour (but not always) from white, to blue, to red. Sometimes this may be painful or cause a tingling sensation during the event. Symptoms of a Raynaud’s attack can last from a few minutes to several hours.
Approximately one-third of people with lupus will experience Raynaud’s phenomenon. In people who have Raynaud’s, the small blood vessels in the extremities are over-sensitive to changes in temperature. This causes a Raynaud’s attack where the toes/feet sometimes change colour (but not always) from white, to blue, to red. Sometimes this may be painful or cause a tingling sensation during the event. Symptoms of a Raynaud’s attack can last from a few minutes to several hours.
If you would like to learn more about Raynaud’s phenomenon, how it is diagnosed and what steps you can take to prevent attacks, take a look at our blog article HERE.
Vasculitis
Vasculitis is a range of conditions in which the blood vessels become inflamed. This can be painful with raised red patches on the legs or there may be small red or black lines around the nails. It can sometimes lead to ulcers on the feet or legs. If you have any of these signs or symptoms then you should seek medical advice. It the toes appear to be black, medical help is required immediately.
To learn more about the various forms of vasculitis, how it is diagnosed, and the treatments, please visit the Vasculitis UK website, HERE.
Erythromelalgia
Erythromelalgia refers to when the hands and/or feet become intensely red, hot, and painful due to dilated or inflamed blood vessels. The affected extremities usually feel better with cold and worse with warmth. This is just the opposite of people who have Raynaud’s phenomenon. You can learn more about the condition and how to manage it HERE.
“I like to use vapour rub on my feet at night. It keeps the skin soft and cools the feet.”
Nails
 Toenail problems are a common occurrence in people with lupus with many possible abnormalities and potential causes. During medical consultations, these problems may be overlooked as there are often other priorities to discuss. However, it is important to discuss these with your consultant or specialist nurse.
Toenail problems are a common occurrence in people with lupus with many possible abnormalities and potential causes. During medical consultations, these problems may be overlooked as there are often other priorities to discuss. However, it is important to discuss these with your consultant or specialist nurse.
For information about the various nail abnormalities that can occur and advice on taking care of your nails, please take a look at our blog article HERE.
“Ensure nails are kept short. I always soak mine for about ten minutes to make them softer. Cut nails straight across and file. Check toes whilst you are doing this and report in-growing toenails to your podiatrist.”
Skin
Shape changes in the front of the foot and the toes can create pressure sites that develop corns and calluses (hard skin). If not treated appropriately, these may develop into areas of ulceration, and so it is advisable to request guidance from a registered podiatrist. Some medications can also have an effect on the skin and underlying tissues, making them more vulnerable to damage and infection.
Some of the medications commonly used to treat lupus (e.g. immunosuppressants such as azathioprine, methotrexate or mycophenolate mofetil) affect the body’s resistance to bacterial, viral (verruca) and fungal (athletes foot) infections. Similarly to nail problems, issues like this may be overlooked during medical consultations but it is important to tell your consultant or specialist nurse about them.
Athlete’s foot is a fungal infection characterised by itchiness and sometimes white and ‘wet’ skin between the toes or flaky redness on other areas. The fungus also breaks down the skin’s natural barrier to bacterial infections and these in turn can be severe. Athlete’s foot can be treated with medications – spray, powder or cream but it is best to get an accurate diagnosis first.
You can view images of some common foot problems and access information about managing them on the NHS website HERE.
What you can do to look after the skin on your feet;
- Wash and examine your feet for damage or problems every day.
- Keep your feet clean and dry them carefully afterwards (especially between your toes).
- Look for blisters or pressure sores. Change your shoes or get professional advice if these signs of stress develop.
- Any dry skin should be kept moist with a good moisturising cream to prevent cracks from occurring.
- Professional guidance should always be sought about self-treatment of hard skin and corns – DO NOT use pedicure blades, corn plasters and paints on these areas.
–
“It is vital to check our feet daily for signs of problems such as cold feet or some other change such as increased pain, heat, redness, discharge or smell. These changes need to be reported to an on-call podiatrist as soon as possible.”
“I was advised to use a prescribed heel balm to reduce hard skin. We should not use strong preparations such as corn plasters as these may make our skin ulcerated and lead to further problems.”
Neuropathy
 Some people may experience problems with the nerve supply to their feet, known as peripheral neuropathy. This can be caused by inflammation of the small blood vessels that supply the nerves, damaging them and thus leading to abnormal nerve function. Typical symptoms are numbness and tingling of the feet. This can feel like a “pins and needles” sensation, and can sometimes be associated with burning pain or pain that feels like an electrical sensation that comes and goes. Often the pain is worse at night when the person is in bed, causing difficulty sleeping. It occurs in 10 to 20% of people who have SLE.
Some people may experience problems with the nerve supply to their feet, known as peripheral neuropathy. This can be caused by inflammation of the small blood vessels that supply the nerves, damaging them and thus leading to abnormal nerve function. Typical symptoms are numbness and tingling of the feet. This can feel like a “pins and needles” sensation, and can sometimes be associated with burning pain or pain that feels like an electrical sensation that comes and goes. Often the pain is worse at night when the person is in bed, causing difficulty sleeping. It occurs in 10 to 20% of people who have SLE.
If it occurs abruptly and severely it is treated with steroids. However, in most people it comes on very slowly and steroids may not be that helpful. If the symptoms are mild, it may not need to be treated at all, but if the discomfort is severe enough, medications that can reduce nerve pain are prescribed. There are many different medications that can be used including opioids such as tramadol, antidepressants such as nortriptyline and duloxetine, and antiepileptic medicines such as pregabalin.
You can learn more about peripheral neuropathy on the NHS website HERE.
What expert help is available?
 Podiatrists can assess your foot structure and the blood and nerve supply. They provide care for common foot problems, advice on footwear and provide insoles (orthoses) in order to relieve foot pain and improve the alignment of the joints. They can also provide management of infections and acute foot problems such as ingrowing toenails.
Podiatrists can assess your foot structure and the blood and nerve supply. They provide care for common foot problems, advice on footwear and provide insoles (orthoses) in order to relieve foot pain and improve the alignment of the joints. They can also provide management of infections and acute foot problems such as ingrowing toenails.
It is important that anyone treating your foot problems is aware of all the medications you are taking so that they can manage any potential problems appropriately.
Podiatrists who work for the NHS are required to register with the Health and Care Professions Council (HCPC) in order to practice. If you see a podiatrist privately, you can check registration online HERE.
Availability of NHS podiatrists does vary in different areas but people with lupus should be able to access this service regardless of age. If you are unsure then ask your consultant or specialist nurse. You can find podiatry services near you HERE.
“I self-referred to a NHS podiatrist for advice for the care and management of my feet. The podiatrist will check the pulses in our feet and ankles and will scan to check circulation. These are vital checks as having lupus may bring with it further complications such as Raynaud’s phenomenon and small fibre neuropathy. If we can’t ‘feel’ our feet due to poor circulation or reduced feeling of hot or cold this is dangerous and may lead to further complications. The podiatrist will also check foot and toe alignment. Having very rough skin on our feet will indicate where we put the most pressure when walking.”
***Please note that this article is written for informational purposes only and should not be a substitute for professional medical advice or treatment. Do not delay seeking or disregard medical advice based on information here. Always seek the advice of your local family physician or other qualified health professional before starting any new treatment or making any changes to existing treatment. It is also advisable to consult a medical professional before making any changes to diet or starting complementary remedies, which may interact with other medications.***
Thank you so much to everyone who submitted their tips and experiences for this month’s topic. We’re sorry if we weren’t able to use your comment in the article this time.



 ©2024 LUPUS UK (Registered charity no. 1200671)
©2024 LUPUS UK (Registered charity no. 1200671)