Testing for Lupus
This site is intended for healthcare professionals as a useful source of information on the diagnosis, treatment and support of patients with lupus and related connective tissue diseases.
Introduction
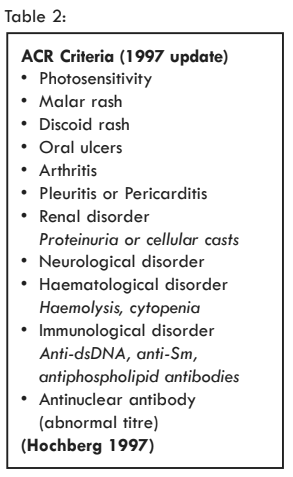
A diagnosis of lupus is based on the patient’s symptoms and results of investigations. Although criteria for lupus exist, e.g. American College of Rheumatology (ACR), they have been developed for research and do not always work well in day to day practice. Investigations include blood tests and imaging studies and aim to help make a diagnosis and determine how widespread and severe the lupus is. Blood tests for autoantibodies are particularly important. Lupus is one of a number of related autoimmune conditions, such as rheumatoid arthritis or Sjögren's Syndrome, and sometimes a lupus patient ‘overlaps’ with one of these.The reasons for performing tests include:
• Providing information to allow a diagnosis to be made
• To discover the presence of other medical conditions that the patient may have
• To assess the severity and extent of disease
• To monitor disease activity and to look for the side effects of treatments
• To try to predict the future (prognosis)
Tests vary on how useful they are depending on the clinical setting and the type of test, however, understanding the importance of a particular result for an individual patient is a key part of managing lupus. Some tests just apply to a part of the body, for example, kidney tests or a chest X-ray, while others reflect problems with the immune system that lie at the heart of the disease. Tests also vary in how available they are, their cost, and how long it takes to have a result.
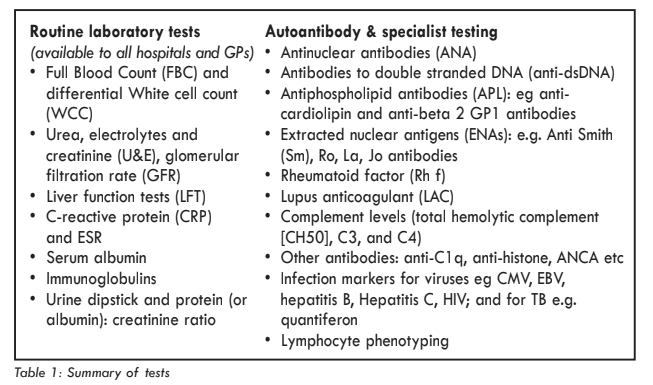
Routine Laboratory Tests
Routine laboratory tests are an inexpensive way of supporting suspicion of an inflammatory process such as lupus and indicating that further investigation is required. They are also useful in monitoring the level of disease activity and progression in patients already diagnosed with lupus, identifying specific organ involvement (e.g. lupus nephritis) and for the guidance of safe treatment with potentially toxic medications. Patients on immunosuppressive drugs (such as methotrexate, mycophenolate mofetil, azathioprine, cyclosporine and tacrolimus) should have regular FBC, U&E and LFT, and some drugs are monitored by assessing the level in the blood e.g. tacrolimus or mycophenolate mofetil. Tests are more frequent when a drug is started or changed, then less frequently e.g. every 8-12 weeks. Regimens for drug monitoring are agreed between the hospital and general practitioner and will vary, however, depending on the drug/dose. It is always helpful for patients to be aware of their test results should communications between clinics be delayed.There are now national guidelines, for example, those published by the British Society of Rheumatology for both lupus and for the monitoring of drugs used in rheumatology that are freely available online through the BSR website. Test results are always important and sometimes require urgent action or discussion with a rheumatologist e.g. the presence of low white cell counts (leucopenia).
See chapter - BSR Guideline for the Management of SLE
Full Blood Count (FBC)
Lupus patients may demonstrate depletion of any or all blood cell types, cytopenias. Anaemia reflects a reduced red cell number and is typically normochromic and normocytic (the anaemia of chronic disease) but may be microcytic due to iron deficiency (this may be secondary to NSAID/steroid induced GI bleeding). In addition, macrocytosis may be caused by megaloblastic anaemia such as in methotrexate-induced folate deficiency (hence concurrent administration of folic acid is recommended with methotrexate treatment) or from administration of azathioprine. When assessing the relevance of MCV in anaemia the variation from the mean red cell size measured by red cell distribution width (RDW) can give additional guidance. For example, MCV may be normal but RDW increased where there is a combined picture (e.g. haemolysis and iron deficiency) due to populations of both large and small red cells respectively.Haemolysis may give a microcytic anaemia with spherocytosis but, if compensated, may lead to a raised MCV secondary to a reactive reticulocytosis (large immature red cells with prominent ribosomal RNA). The Coombs tests identifies an antibody cause for the haemolysis. If haemolysis is suspected clinically (jaundice, dark urine), a haemolytic screen should be undertaken, including lactate dehydrogenase, blood film to identify reticulocytes and haptoglobin levels which, in transporting free Haemoglobin to the spleen, will be diminished if red cell lysis is occurring in the circulating blood volume.
Haemolysis in lupus may occur in association with thrombocytopenia, a reduced number of platelets (also known as thrombocytes). This is most commonly recognised as thrombocytopenic purpura (TTP) or haemolytic uraemic syndrome (HUS) which can be classified under an umbrella diagnosis of Thrombotic Microangiopathic Haemolytic Anaemia (TMHA). Although traditionally thought to be rare, there is now recognition that under-diagnosis is common and its role in lupus is gaining increased interest in the literature. It should be considered in patients presenting with these features alongside fever and neurological or renal involvement. A moderate thrombocytopenia (PLT~100) is also seen in APS. In lupus TMHA can be caused by an antibody to ADAMTS 13.
Other blood cell populations affected by lupus include leukocytes or white cell, which are typically diminished, lymphopenia being the most common picture. One must also be cautious of a decreased lymphocyte count in Afro Caribbeans – which might be the result of increased lupus activity or merely the result of an ‘ethnic’ lymphopenia. This is particularly important given the increased prevalence of lupus in such populations.
Iatrogenic leukopenia is also common, for example, with immunosuppressive drugs such as cyclophosphamide, which may result in acute or chronic myelosuppression. Neutropenia is typical and may be clinically important, but a diminution in total WCC may also reflect lymphopenia, with relative preservation of the neutrophil count. In this situation, it may be inappropriate to reduce or stop a cytotoxic drug as the lymphopenia may be an indicator of enhanced lupus activity. If in doubt, specialist advice should always be sought.
Azathioprine rarely causes a severe neutropenia in patients with a deficiency of thiopurine methyltransferase (TPMT), an enzyme responsible for s-methylation of thiopurines. Although TPMT activity and genotype can be tested for before commencing the drug, this is not essential provided there is appropriate FBC monitoring in place. In addition, patients with Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency are at risk of haemolysis when treated with dapsone or sulfonamide antibiotics. These deficiencies can also be screened for prior to commencing dapsone but are not essential if monitoring is in place. Mycophenolate mofetil can cause anemia, leucopenia or thrombocytopenia. It can be difficult to tell if reduced blood counts reflect disease activity or drug toxicity.
Consequently, WCC is most usefully interpreted in light of total and differential WCC, paying attention to the trend in white cell count and other clinical features such as fever or local symptoms of infection, particularly when patients are on immuno-suppressive medications. Immunosuppressives may also cause a selective lymphopenia which can be missed if the total white count is normal, but infer an increased infective risk.
Urea & Electrolytes (U&Es)
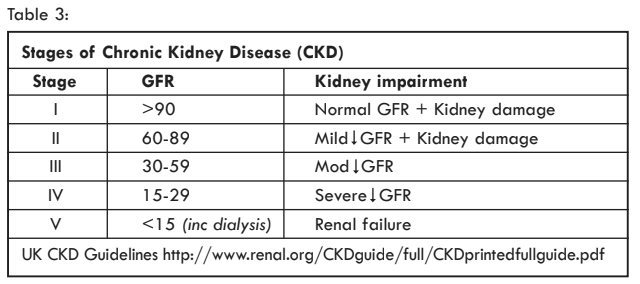
Renal complications in lupus patients are usually first detected by abnormal urine tests, especially proteinuria. Kidney function is assessed by Glomerular Filtration Rate (eGFR) calculated from creatinine levels (compensating for race, age, gender and body size – see Table 3). More acute changes in renal function are best monitored with creatinine and electrolyte levels. It is important to be aware that serum creatinine can be in the ‘normal’ range but significant kidney failure may be present. The eGFR has been introduced to try to improve on this. It is often reported as greater than 60ml/min (i.e. normal), but for a younger person this can disguise a major fall in kidney function, say from 100 to 70ml/min. Sequential measurements of creatinine can alert the physician if there is an upward trend.In the majority of cases, lupus nephritis is detected by the presence of urine abnormalities with a ‘normal’ eGFR. Any unexplained urine abnormality should alert the physician to the possibility of renal involvement. Less commonly, nephritis presents with acutely elevated creatinine levels (acute kidney injury). Rapid increase in creatinine levels in a lupus patient known to have chronic kidney disease (e.g. a persistently low eGFR), may also signify progression from background lupus activity to more severe renal damage. Monitoring of blood pressure is also important in such patients since thrombosis of the renal vasculature can lead to occlusion and, consequently, mesangial ischaemia which itself can trigger angiotensin II secretion and subsequent hypertension.
It is also important to be aware of the large number of therapies in lupus that can cause renal impairment. Treatment with NSAIDs and ACE inhibitors can lead to decreased ability to regulate renal blood flow in response to haemodynamic compromise by impairing afferent vasodilation and efferent renal arteriole constriction respectively. These drugs should be used with caution if renal perfusion could be reduced.
In any case, new derangement of renal function should be carefully considered and represents an opportunity to recognise acute and early chronic renal impairment so should be carefully monitored with further investigation where appropriate. Techniques available include laboratory urine biochemical analysis and microscopy for signs of glomerulonephritis or nephrotic syndrome. Any patient who has suffered from renal disease with their lupus should have life-long review of U&Es, BP and urinalysis 3-6 monthly (more frequently during an acute episode).
Urinalysis
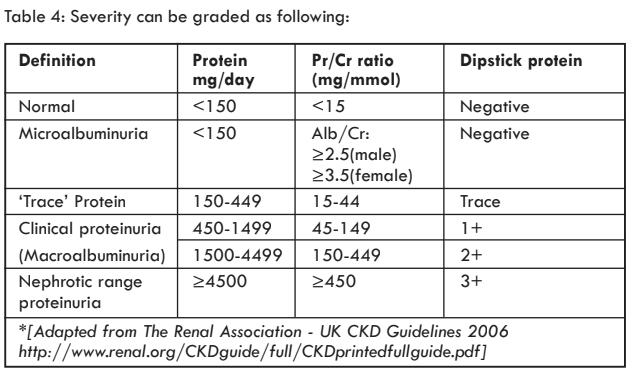
Urinary dipsticks test for protein, blood, leukocytes, nitrites and pH. Positive results of any of these tests can signify renal pathology but contaminating causes (e.g. UTI or menstrual blood) should be kept in mind when appropriate. In such situations, a careful history will often suggest a cause. It is important, however, not to dismiss an abnormal dipstick too readily until the possibility of renal pathology can be confidently excluded.The presence of haematuria is of greater significance if red cell casts can be identified by microscopy, signifying glomerulonephritis which may represent a flare of lupus nephritis, but in practice these are often not looked for.
Proteinuria is usually measured by the protein (or albumin) creatinine ratio and 24 hour collections (result given as mg/day) are now less commonly collected. The PCR is best assessed on a sample from the first urine void in the morning. A normal PCR is less than 15mg/mmol and any values above this that are consistent should raise suspicion of nephritis. The threshold for a kidney biopsy is a PCR of 50 but can be lower if other abnormalities are present. Biopsy is also recommended for persisting blood or leucocytes in the urine or an unexplained fall in eGFR.
Liver function tests (LFTs)
LFTs derangements are usually mild and non-specific but are not uncommon in lupus patients, which can be due either to autoimmune liver involvement or treatments employed. Hepatitis with elevation of parenchymal liver enzymes is seen with NSAIDs (especially diclofenac), aspirin and methotrexate and can also be associated with azathioprine or hydroxychloroquine. Corticosteroids can derange LFTs by causing a fatty liver.Low albumin may reflect proteinuria associated with renal disease or poor nutritional status in patients with severe multi-system disease. In addition, pancreatitis can occur in lupus patients, potentially following steroid treatment and justifies measurement of amylase levels where there is epigastric pain or malabsorption.
Persistently deranged LFTs should prompt consideration for further investigation with abdominal ultrasound and liver biopsy.
C-Reactive Protein (CRP) & Erythrocyte sedimentation rate (ESR)
CRP is an acute phase protein which has been used as an inflammatory marker with a short half-life which responds quickly to the development of an inflammatory state – CRP can be substantially raised within six hours of infection.The CRP level is, however, not typically elevated by active lupus and remains a useful indicator of an inflammatory response to an infection. There are, however, occasions when lupus flares alone can lead to a moderately elevated CRP (e.g. Serositis) even in the absence of infection.
ESR describes the height of red cells that settles in a defined unit of time – usually one hour. Normal upper limits are 15mm in men and 20mm in women and are typically increased in an inflammatory response such as that seen in lupus or to infection. A patient with ‘active’ lupus will generally have a significantly elevated ESR (often >50), often in the absence of raised CRP as mentioned above. ESR is, however, an indirect measure of all acute phase proteins and can be elevated in many situations, including anaemia and hypergammaglobulinaemia (common in Sjögren’s Syndrome). ESR responds less rapidly than CRP and is also slow to change with alterations in the inflammatory response.
Infection serology
The presence of chronic infections can influence the course of lupus and complicate its therapy. As a routine, tests are usually performed for hepatitis B, hepatitis C and HIV. Tuberculosis (TB) testing is performed for those considered higher risk. Lupus can result in a falsely positive VDRL (venereal disease research laboratory) test for Syphilis. This is due to cross reaction of the test antibody and such results must be interpreted in light of the clinical context with an accurate history of sexual partners/activity. A positive result should be followed up by more accurate tests such as Treponema Pallidum Haemoglutination Assay (TPHA) and the possibility of lupus should be considered. Patients who are immunosuppressed are at risk of less common infections such as CMV for which there are now good blood tests.Specialist investigations
The literature describes over 100 different auto-antibodies in the sera of lupus patients. These may result from the loss of tolerance to self-antigens, including nuclear antigens or cell surface fragments such as phospholipids. Soluble antigens e.g. complement, may also be targeted. The identification of these antibodies using the following techniques has assisted with the formalisation of diagnosis of lupus:• Enzyme linked Immunosorbent assay (ELISA)
• Radioimmunoassay e.g. Farr assay
• Participation assay
• Passive agglutination
• Complement fixation
• Immunofluorescent assays
Auto-antibodies are polyclonal - they are of varying ‘isotypes’, with a range of affinities and avidities to their target antigens. The result is that diagnostic tests vary in their ability to identify the slight variations in these antibodies. Given the hypothesis that autoantibodies might be directly responsible for the pathogenesis of lupus, this polyclonality may also influence disease severity through differences in affinity and avidity of autoantibodies to their target antigens (antibodies with greater affinity might be more destructive). Class switching to IgG is thought to be more harmful than IgM and positive IgG antibodies are generally of greater significance than the IgM isotype.
Of these autoantibodies, most are detectable in fewer than 30% of lupus patients and the tests discussed further are the limited number more commonly investigated. ANA is the most sensitive test for lupus whereas anti-dsDNA and anti-Smith antibodies are more specific.
ANA - Antinuclear Antibodies
Nuclear antigens are those that have roles in cell cycle function, transcription, translation or as structural proteins. Antibodies against any nuclear antigen are known as antinuclear antibodies (ANA). There are two types of ANA test:• Direct immunofluorescence against these antibodies are reported as a titre, such that high values (> 1:320 – corresponding to a positive signal when more diluted) are more likely to represent true positives than lower titres (1:40). The best substrate are a cell line ‘Hep-2 cells’, which have large nuclei. A positive result should be followed by characterisation of the staining pattern (see below).
• ELISA (or other ‘solid phase’ test). These have become popular because they can be automated and are less observe dependent. They usually comprise a ‘soup’ of the more common lupus autoantigens. They will miss ANAs targeting less common autoantigens and are more subject to ‘false positive’ results. They are often the first test a laboratory performs, but if negative and suspicion for lupus remains, a direct immunofluorescence test should be requested. A positive result should result in testing for the individual components in the ‘soup’ and at least one should be positive.
In selected populations, when ANA titres are high, sensitivity of this test for lupus can approach 100% and specificity about 90%. However, false positives are common, for example, in other connective tissue diseases - and particularly in unwell elderly patients. ANA’s are also occasionally seen in subacute bacterial endocarditis, pregnancy, HIV, liver disease, malignancy and Type 1 diabetes mellitus.
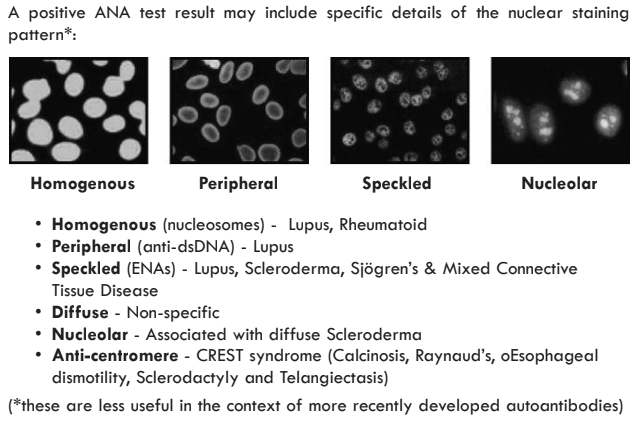
ANA is a test with a high sensitivity but with a low positive predictive value since it can be false positive in both normal individuals and those with other connective tissue diseases and so is best applied to those patients with a high predicted risk. Serial measurements are not recommended as there is poor correlation with disease progression. In addition, lupus-like syndromes are recognised in the absence of positive ANA (other serology such as anti-Ro or La may be positive) and patients with previously sero-positive lupus may not be consistently positive for ANA.
Anti-dsDNA - Anti Double Stranded Antibody
One of the most useful types of anti nuclear antibody to test for in lupus is anti-dsDNA antibodies. These are antibodies found in the cell nucleus, bound preferentially to DNA and are associated with a predisposition to developing lupus. These are commonly detected by: dsDNA ELISA and crithidialucillae immunofluorescence. They are included in the ANA ELISA test.Whilst many patients with active untreated lupus produce anti-dsDNA antibodies, the sensitivity of this test is limited, with approximately just 60% of patients with lupus having a positive test result. Testing is, therefore, not recommended when ANA is negative, where the probability of lupus would be expected to be low. It is, however, one of the most specific autoantibody tests in lupus – particularly when titres are high and where the antibodies are IgG isotype complement fixing antibodies (rather than IgM antibodies, which precede class switching and are associated with an immature response to antigen).
It has been suggested that anti-dsDNA antibodies might be implicated in the pathogenesis of lupus. It has been shown (using activity indices such as SLEDAI/BILAG), that levels of some anti dsDNA antibodies appear to correlate with disease activity in lupus and predict flares of lupus nephritis. Furthermore, DNA-antibody complexes have also been isolated from sites of renal damage.
Lupus patients might be expected to be “sero-negative” for anti-dsDNA antibodies early in disease, post-treatment and when in clinical remission. Anti-dsDNA antibodies are also of less use in subacute or discoid lupus. Isolated negative samples cannot, therefore, be used to exclude lupus. Furthermore, it is recognised that not all anti-dsDNA antibodies are associated with lupus activity - low titres of anti-dsDNA antibodies are sometimes seen in patients with myeloma and, occasionally, those with other autoimmune diseases such as rheumatoid arthritis.
The presence of anti-dsDNA antibodies is generally useful in the diagnosis of lupus, particularly in the context of high clinical suspicion. However, anti-DNA antibodies are heterogenous with different binding characteristics such that some anti dsDNA antibodies are not associated with clinical symptoms. Anti-dsDNA antibody titres can also be used to guide therapy. In some circumstances, increasing corticosteroid dosage in response to a rise in anti-dsDNA antibodies may pre empt a clinical flare. However, in most cases, therapeutic decisions should be based on clinical symptoms and signs or other abnormalities, indicating end-organ damage, rather than on changes in anti dsDNA titre or complement levels alone. Levels of disease activity can often be readily monitored by following a trend in lymphocyte count, climbing ESR or a fall in complement components.
A positive crithidia lucillae immunofluorescence test has a higher specificity for anti- dsDNA but lower sensitivity and is used when more confidence in the specificity of the routine anti-dsDNA test is required.
Extractable Nuclear Antigens ENA
These are soluble components of the nucleus and cytoplasm that may be targeted by autoantibodies in connective tissue disorders such as lupus. The presence of a speckled pattern ANA would suggest the need for the following more specialised tests. These antigens are also included in the routine ANA ELISA.Anti-Smith (Anti-Sm) antibodies
Anti-Smith antibodies in high titres are considered pathognomonic for lupus and are included in ACR criteria. They are, however, detectable in as few as 20-30% of lupus patients and are seen in low titres in other diseases. They are most frequently seen in Black Americans and rarely in other ethnic groups. Anti-Smith antibodies are targeted against proteins that form part of the common core of U(1,2,4,5) small nuclear ribonucleoproteins (snRNP). Antibodies to anti-Sm(D) are considered most specific to lupus, particularly anti-Sm D1 which are strongly associated with lupus nephritis and correlate with disease activity. Neuropsychiatric involvement is also more frequently recognised.Anti-Ribosomal RNP antibodies
These antibodies against proteins associated with the common ribosomal core e.g. U1, protein A and C are seen in approximately 30% of patients with lupus and are associated with the presence of Raynaud’s phenomenon, whilst also usually indicating milder renal disease.Anti U1 snRNP
Anti U1 snRNP is most closely linked to MCTD but is also seen in lupus. Its sensitivity, however, is poor and it may be present as part of an overlap syndrome. Testing for anti U1 snRNP should be limited to those with positive ANA, where there is suspicion of lupus/MCTD.Anti-Ro (anti-SS-A) and Anti-La (anti-SS-B)
Whilst very common in primary Sjögren’s Syndrome, particularly in the presence of extra-glandular features, anti-Ro and La are also well recognised in lupus where they may be associated with a secondary Sjögren’s Syndrome with symptoms of Sicca. Antibodies to Ro, a 60 KDa RNA binding protein, occur in up to 50% of lupus patients, especially in the presence of leukopenia, congenital heart block and photosensitive skin rashes.Antibodies to the 48KDa La antigen occur in 10-15% of lupus patients and predict late onset lupus, but are rarely seen in the absence of anti-Ro. Anti-Ro and La are also recognised in rheumatoid arthritis and polymyositis. Hence, neither is specific for lupus but may be useful in the absence of anti-dsDNA.
Anti-Histone antibodies
50-80% of lupus patients may have antibodies to Histones (which act as interacalated spools around which DNA wind). This may be to complete Histones or subfractions H1, H2a, H2b, H3 and H4. Specific correlation has been made to drug induced lupus for which there is good sensitivity, but poor specificity Histone antibodies cannot be used to distinguish between drug induced lupus and systemic lupus, however, drug induced antibodies are usually IgM and may occur without clinical manifestations. Titres usually diminish with resolution of drug induced lupus. This test is probably most useful when interpreting a known history of exposure to relevant drugs e.g. procainamide or isoniazid.Rheumatoid factor
Rheumatoid factors are usually IgM antibodies directed against the Fc region of human IgG. They occur in 40% of lupus patients but are also positive in a wide range of rheumatological conditions and in the normal population – particularly in older patients. There is also an association with infection, pulmonary disease, PBC, colon cancer or leukaemia. High Titre Rheumatoid factor is a common feature of Type II cryoglobulinaemia (see below).Lupus anticoagulants and the antiphospholipid antibodies (APL)
The presence of these antibodies confer an increased risk of arterial or venous thrombosis and certain other complications in lupus patients. When these events occur with APL but in the absence of lupus, the term antiphospholipid syndrome (APS) is used. Diagnosis of the Anti-phospholipid syndrome itself requires clinical evidence of thrombosis in association with the above antibodies. A positive lupus anticoagulant should be re-tested after twelve weeks to confirm antibody persistence. Lupus patients without APL still have an increased thrombus risk. Antiphospholipid antibodies are antibodies to negatively charged phospholipids and include the lupus anticoagulant and anticardiolipin antibodies (ACA). The presence of APS is also associated with a significant rise in pregnancy related complications.There are three types of test:
• The lupus anticoagulant (LAC) They are so named because in vitro they inhibit the prothrombinase complex, resulting in a prolongation of clotting assays such as the activated partial thromboplastin time (aPTT), the dilute Russell viper venom time (dRVVT), the kaolin plasma clotting time (and, rarely, the prothrombin time)*. In vivo this leads to an increase in thrombotic tendency resulting in, for example, deep venous thrombosis or pulmonary embolus. These clotting tests cannot be performed on patients receiving anticoagulants.
• Anti-cardiolipin antibodies (ACL). Both IgG and IgM isotypes are measured.
• Anti-beta 2 GP1 antibodies. Both IgG and IgM isotypes are measured as these tests represent the antigenic target of ACL and are more specific.
The strength of association with clinical thrombotic events is lowest for ACL (lower for IgM than IgG), intermediate for anti-beta 2 GP1 and highest for LAC.
Cryoglobulins
Cryoglobulins are abnormal proteins that precipitate reversibly at low temperatures and can result in blockage of blood vessels, with subsequent purpura and nephritis. Many autoantibodies seen in lupus behave in this manner. Cryoglobulins may be simply tested by cooling serum in the laboratory. It is necessary that samples be taken directly to the laboratory at 37° (e.g. in a cup of warm water) where the sample can be immediately centrifuged to isolate and refrigerate the serum and hence this test can only be performed in a specialist centre by arrangement with the lab.Complement
Complement proteins (both free and membrane bound), form an important part of the innate immune defence and are activated by:a) Classical pathway (immune complexes or CRP)
b) Alternative pathway (bacteria or viruses)
c) Mannose Binding Lectin (MBL) pathway (carbohydrate structures on micro-organisms)
Physiological roles of complement include opsonisation of bacteria, attraction and activation of inflammatory cells, solubilisation of immune complexes and formation of the membrane attack complex with resultant cell lysis. Deficiency in complement components predisposes to infection, particularly with pyogenic organisms. Deficiency in the classical pathway components specifically, is associated with lupus. This is recognised in the context of inherited complement deficiency and also in the presence of antibodies to specific complement components. Such findings have led to the hypothesis that complement deficiency is important in the pathophysiology of lupus. This is supported further by the recognition of tissue inflammation and organ damage with activation of certain components of complement (e.g. C1q), in tissue.
Anti-C1q antibodies
C1q is the first component in the classical activation pathway of complement and is thought to be particularly important in the context of severe systemic lupus and lupus nephritis - indeed, antibodies to C1q are closely correlated with damage to the kidneys and more severe lupus activity. C1q may have a role to play in immune complex clearance - it is thought that tissue injury may arise from defective immune complex clearance as a result of hypocomplementaemia. Defective clearance of apoptotic cells may also underlie such damage. An increasing C1q antibody titre in lupus patients can be used to predict a flare in lupus nephritis - this is of use in both screening and follow-up of individuals susceptible to development and progression of lupus nephritis. An association is also recognised between C1q antibodies and hypocomplementaemic urticarial vasculitis syndrome (HUVS).C3 and C4
All three complement pathways converge at C3, ‘the common pathway’. Persistently low C3 levels are seen in lupus patients and may be due to consumption by immune complexes. Binding of the cleavage product (C3b) to micro organisms and immune complexes results in activation of the terminal complement components, with activation of the membrane attack complex (MAC- C5b-9).C4 is highly polymorphic and encoded by two genes (C4A and C4B) which differ considerably with regards to their antigenic binding activities. Complete C4 deficiency requires homozygosity for the rare double null haplotype C4AQ0,BQ0 and predisposes to infection and lupus. Partial C4 deficiency is more common and associated with lesser auto-immune phenomena.
Laboratory measurement of acute consumption of C3 and C4 in this scenario can be used to anticipate a lupus flare. Alternatively, a surge in complement degradation products (C3d and C4d) also demonstrate disease activity. It is recognised that homozygous genetic deficiencies in C3 and C4 also predispose to lupus.
CH50
The total haemolytic 50% (CH50) assay represents a functional assay of the activity of the entire complement system, by measuring the ability of a test sample to lyse 50% of a standardised suspension of sheep erythrocytes coated with anti- erythrocyte antibody. This assesses the classical pathway of activation and also terminal components of the complement system. The degree of lysis is proportional to the amount of complement in the test solution.CH50 is not routinely measured in most laboratories, but it may be useful in the detection of genetically determined complement deficiency (e.g. C1q or C2).
Immunoglobulins and lymphocyte phenotyping.
There are three classes of antibody in the blood, IgG, IgM and IgA and these are part of the healthy defence against infection. In active SLE, IgG levels may be raised which reflects non-specific immune activation. After drugs that target B cells, such as belimumab, rituximab or mycophenolate, immunoglobulin levels can fall increasing the risk of infection. Lymphocytes can be subdivided according to markers on the cell surface, e.g. B cells, T cells, CD4/CD8 etc. Rituximab depletes B cells from the blood and measuring B cell counts can be helpful for certain patients when monitoring this treatment. Selective depletion of other cell subsets e.g. CD4+ T cells can occur as a result of lupus activity or medication and render the patient at high infection risk.
Conclusion
Whilst lupus is a predominantly clinical diagnosis, developments in more specialist tests, particularly auto antibodies, strengthens the role of investigations in diagnosis. Additionally, the multi-system nature of lupus demands close vigilance of all organs, reinforcing the importance of routine investigations which, alongside serology, are useful in monitoring disease activity. Results should be interpreted in the context of the clinical picture. Better understanding of the methodology and limitations of investigations often facilitates such an approach.Prof David Jayne
Professor of Clinical Autoimmunity
Dept. of Medicine
University of Cambridge
Honorary Consultant Physician
Addenbrooke’s Hospital
Cambridge CB2 2QQ
Revised and updated from 2009 edition by Dr Richard Lee and Prof Kevin Davies

 ©2024 LUPUS UK (Registered charity no. 1200671)
©2024 LUPUS UK (Registered charity no. 1200671)