Complementary and Alternative (CAM) Treatments of Lupus
This site is intended for healthcare professionals as a useful source of information on the diagnosis, treatment and support of patients with lupus and related connective tissue diseases.
Introduction
Complementary and Alternative (CAM) treatments are a group of diverse medical and health care systems, practices and products that are not presently considered to be part of conventional medicine. Complementary Medicine is used in addition to conventional or mainstream medicine, whereas, Alternative Medicine is used in place of it. Most people use therapies as Complementary Medicines with true Alternative Medicines being less commonly used.This definition of CAM hides its overlap with modern medicine. Treatments widely used as mainstream medicines could be considered as CAM in their original form. Aspirin was isolated from willow tree bark, atropine from the plant Bella donna, Digoxin from Foxglove amorphine, from the poppy Papaver somniferum. Alternative healthcare systems such as Ayurvedic, meditation and relaxation techniques, emphasise the interplay between psychological factors and the immune system. Stress can trigger immune mediated conditions such as Psoriasis and may affect lupus disease activity.
The link between these “natural” products and modern medicine makes the use of CAM appealing. Although tempting to extrapolate from these examples, it is important to review the evidence for the most widely used CAM products to determine whether other natural products are potentially medicinal.
Background
What is CAM used for?About 30% of all CAM usage, the majority, is for musculoskeletal conditions, especially back and joint pain. The most frequently used CAM are non-vitamin, non-mineral products such as omega 3 oils, ginseng, deep breathing, meditation and yoga.
What drives the use of CAM?
People who use CAM aim to improve their health and wellbeing. Unhappiness with side effects or effectiveness of conventional treatments are important factors in usage. Some patients believe that using CAM provides a more natural or holistic approach, allowing greater control over their condition and its management.
CAM use in SLE
Evidence suggests lupus activity in patients who use CAM is the same as those who do not. However, perhaps over 50% of lupus patients use CAM and do so because they believe they have worse disease activity than those who do not. While current disease activity may be similar, SLE patients who use CAM may, however, have worse historic organ damage and greater pain and incur greater direct health costs. Some CAM users may feel less secure about their condition and see their doctor more frequently or utilise other resources more avidly. They may also be unhappy with conventional treatments or want to augment these treatments.
CAM Therapies: classified and examined
Which medical and health care systems, practices, and products can be considered as CAM? In the USA, the NIH (National Institutes for Health) classify CAM therapies into 5 distinct groups, used for simplicity in this text (Table 1) but specific therapies can overlap in more than one group.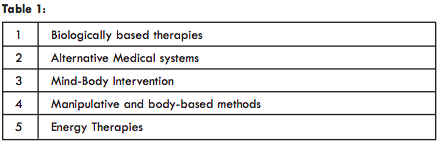
1. Biologically based CAM therapies - Vitamins
Vitamin A comprises a group of compounds including retinol, retinoic Acid and βCarotene. It is essential for healthy skin, gum and skeletal growth and low light and colour vision. Deficiency of Vitamin A is globally common and the leading cause of childhood blindness. Vitamin A is found in animal (cod liver oil, liver) and plant products (carrots, tomatoes, broccoli) so is easy to obtain.Studies of Vitamin A supplementation in human lupus are sparse and numbers small. Dietary intake of Vitamin A may be lower in SLE patients, but blood levels are not. Vitamin A can be associated with regulation of the immune system by its action on reducing pro-inflammatory chemicals (cytokines) while increasing inhibitory ones. This is most evident in lupus animal studies where characteristic lupus-like skin lesions do not develop after treatment with Vitamin A. One human study of 3 lupus patients given Vitamin A showed skin lupus lesions cleared within a week.
Vitamin C supplementation may be associated with reduced cancer risk and may reduce the duration, though not the frequency, of the common cold. It is essential for stress hormone (catecholamine) synthesis, cognitive functions, including memory, and can moderate oxidative stress. This latter role seems to be the key reason that Vitamin C has been used as CAM. Oxidative stress is a process by which reaction of chemicals in the body with oxygen produces short-lived highly reactive free radicals which may promote inflammatory tissue damage. Free radicals may damage DNA, permitting production of the familiar anti-DNA antibodies seen in lupus or affect lipids (“fats”) including cholesterol, allowing oxidative damage and promoting heart disease. Some studies suggest SLE patients have lower levels of protective antioxidants e.g. glutathione, thereby promoting damage and inflammation.
Studies in SLE patients suggest pro oxidant processes which correlate with disease activity are favoured over antioxidant ones. Therefore, it makes some sense to use antioxidants to rebalance this feature of lupus. Supplementation for 3 months with Vitamin C (500mg daily) and Vitamin E (800IU daily) correlates with decreased markers of oxidative stress and lipid oxidation, perhaps suggesting an ability to reduce cardiovascular risk or disease activity.
One clinical trial also studied the association of dietary factors in 279 SLE patients with inactive disease with the development of flares, heart disease, strokes and thrombosis. There was an inverse correla-tion between Vitamin C and crude fibre intake and the development of flares of active disease. A large study of 184,643 women, however, failed to confirm a link between consumption of antioxidants including Vitamins A, C and E and the development of lupus or Rheumatoid Arthritis. Note: Supplementing with Vitamin C rich foods such as oranges, broccoli, tomatoes and whole cereals is a sensible way of achieving the recommended daily intake of 75mg (Women) and 90mg (Men). There is little justification for supplementing with higher strengths unless patients have problems with the bowel or cannot eat normally. Higher doses may interact with drugs, reducing the effect of warfarin or increasing oestrogen levels in those patients taking the oral contraceptive.
Vitamin D is a hormone made predominantly by the action of sunlight on skin. This is important because lupus patients should avoid direct sunlight. Vitamin D receptors are found in organs which process Vitamin D including skin, kidney and Parathyroid Glands but also in immune cells suggesting Vitamin D may affect the immune system. There are two important questions regarding Vitamin D. First, can low Vitamin D cause autoimmune disease? In large epidemiological studies, people who have a higher intake of supplemental Vitamin D seem to have a lower risk of multiple sclerosis and rheumatoid arthritis, which, like lupus, are auto-immune conditions.
Secondly, can low Vitamin D promote worse lupus disease activity? In one study of 177 patients with SLE, low vitamin D was found in 82% of patients and associated with worse disease activity and worse blood test markers such as dsDNA. Another study of 290 SLE patients confirmed these results. Lower Vitamin D3 levels correlated with higher clinical lupus activity including musculoskeletal, skin and kidney disease. In addition, low Vitamin D was associated with higher levels of blood markers such as dsDNA, but not with scores reflecting organ damage.
Vitamin E and other antioxidants
Like Vitamin C, Vitamin E is an antioxidant. Natural vitamin E exists in several forms but only α-tocopherol meets human needs. The required dietary intake is 22.4 units (15mg) for both adult men and women. Vitamin E is found in nuts, seeds, vegetable oils, kiwi fruit, mango and tomatoes. Vitamin E supplements often contain higher than 100 Units, much more than the required daily intake.
Vitamin E may reduce the level of important immune chemical messengers called cytokines. It may also reduce the oxidation of lipids like cholesterol and could potentially reduce cardiovascular disease as a result. Since inflammation is responsible for the widespread tissue damage in lupus and may increase cardiovascular risk, antioxidant vitamins may aid prevention, or delay onset, of the disease while reducing cardiovascular
risk.
Vitamin E also helps stabilize lysosomes, packets of destructive enzymes in some immune cells used to fight microbes. When lysosomes become unstable, their enzymes can damage surrounding healthy tissue. Vitamin E could, therefore, theoretically prevent the onset of
autoimmune damage. The symptoms of lupus-prone mice treated with vitamin E improved. The mice lived longer, immune cell activity was normalized, anti-DNA antibodies were reduced and kidney function improved.
Historically, Vitamin E has been used in the treatment of skin lupus with some anecdotal success but one study of 7 patients demonstrated no benefit. A case report of two patients indicated that topical formula vitamin E improved discoid lupus erythematosus activity.
In more recent studies, 12 SLE patients received 150-300 mg Vitamin E and steroids, while 24 received steroids alone. While markers of oxidative damage (Urinary 8-hydroxydeoxyguanosine) were no different between groups, the levels of dsDNA, which can reflect lupus activity, were lower in the Vitamin E group. Other studies have suggested a similar reduction of the level of autoantibodies in lupus patients. However, it is difficult to draw conclusions from such small studies.
Other antioxidants include N-acetyl Cysteine (NAC). NAC is used in medical situations including preventing oxidative liver damage in paracetamol overdose. It is a precursor of glutathione, a naturally occurring antioxidant whose levels are low in the immune cells of patients with SLE.
Different doses of NAC improved lupus disease activity in patients with lupus kidney disease compared to placebo in one study. NAC was found in higher levels in the immune cells of these lupus patients after treatment while reducing the activity of mTOR, a marker of immune cell function which is often elevated in SLE. Side effects, particularly nausea, were prominent at higher NAC doses (4.8 gm per day). Improvements were also reported in another study of 25 lupus patients given NAC compared to healthy controls. NAC was used for symptoms related to the ADHD Checklist (e.g. “How often do you have problems remembering appointments or obligations?”, or “How often do you make careless mistakes when you have to work on a boring or difficult project?”). Lupus patients improved some of their cognitive/inattention scores on this scale but not the impulsivity scores.
Ginger and Turmeric
Curcuma xanthorrhiza is an extract from ginger with possible immunomodulatory properties including regulation of T-cells and cytokines. It attaches to the VitaminD receptor. In one study, 40 SLE patients were given Vitamin D with either placebo or Curcuma xanthorrhiza. While disease activity improved in all patients, patients given Curcuma xanthorrhiza did not derive additional benefit.
Turmeric is a member of the ginger family. It has claimed benefits in treatment of inflammatory bowel diseases, cholesterol and cancer. An analysis of studies has concluded there is evidence that the active ingredient (Circumin) alleviates joint pains but the studies were small and too few to draw conclusions. One study in Iran looked at whether the regular addition of 500mg Turmeric capsules three times a day with each meal (active ingredient Circumin 21.5 mg per capsule) helped 24 patients with refractory lupus. Patients who took turmeric capsules, but not controls taking identical starch tablets, had reduced blood pressure, protein and blood leakage through the kidneys. Other factors such as steroid or medication changes may have been responsible and the study size was small, limiting any conclusions.
Other Herbal Remedies
Herbalism is the practice of using plants for medicinal purposes. It is not to be confused with the use of plants products which became medicines (see introduction) because most herbal remedies have never undergone formal testing through scientific studies or extended usage. There is mixed evidence for some herbal remedies. For example, Arnica, from the flowering plant Arnica montana (Wolf’s Bane) when applied at 50% concentration in hand osteoarthritis may have similar benefit to ibuprofen gel in pain relief. However, a systematic review of several studies failed to support its use at concentrations below 10% with too little data on higher concentrations for the effects to be clear.
Several proposed herbal products have undergone testing, but the evidence is often of poor quality. The Australian government commissioned a study to evaluate whether herbal remedies could be provided under healthcare schemes and found no evidence of benefit.
Most herbal remedies in the UK and USA are sold as food supplements. As a result, they can evade quality and safety regulations which would apply if they were sold as medicines. There are no standards for the quality of herbal products and no regulation of manufacturers. Some herbal medicinal products such as Cannabis are illegal in some countries or tightly regulated in others, while others are known to be toxic and have caused deaths. Problems with the content of herbal remedies have been reported. Up to 33% of Chinese herbal remedies available in Taiwan were adulterated with conventional medicines to promote their potential effect. The additives include steroids and phenylbutazone, an anti-inflammatory not routinely available in the UK because of toxicity. In another USA study, of 260 Asian patent herbal medications, 32% contained undeclared pharmaceuticals or heavy metals, whereas contaminants including arsenic, mercury and bacteria have also been revealed in widely available herbal remedies. A study of herbal creams in the UK showed that 8 of 11 preparations contained an undeclared potent steroid, dexame-thasone at high concentrations, with potential severe side effects.
Ginseng has been claimed to have health benefits including in Raynaud’s syndrome. In a study of 50 commercial ginseng preparations sold widely, 12% did not contain any ginseng, while 88% contained only between 1.9% to 9.9%.
Ginseng, in common with some other herbal remedies such as St. John’s Wort and Kava, can also interact with conventional medicines. Ginseng can potentiate the effect of warfarin, while gingko biloba can affect the activity of aspirin. These interactions must be borne in mind when discussing medications with a lupus specialist.
Probiotics are non-pathogenic live bacteria and yeast, most commonly the bacteria Lactobacillus and Bifidobacterium, and the yeast Saccharomyces boulardii. The suggested mechanism by which they could work include producing chemicals such as lactic acid, propionic acid and acetic acid which inhibit or change the behaviour of other potentially harmful bacteria. As a result, Probiotics have been promoted as “helping” the immune system. Most probiotic organisms are found in the normal gut, but not all, and the presumed beneficial effects attributed to a particular strain cannot be generalized.
Probiotics have been suggested as a treatment for infections such as antibiotic associated diarrhoea. Drinks containing mixtures of bacteria (for example, Actimel containing Lactobacillus casei imunitass, Saccharomyces thermophilus and Lactobacillus bulgaricus) and those mainly containing single types have both been used with conflicting evidence for their use.
A number of autoimmune conditions may have a link to microbes. Many of the suspected ones involved may reside in the bowel and there is some evidence that gut bacteria in SLE may be altered in composition and proportion.
Lupus animal studies suggest “leaky gut” predates lupus kidney disease. One study suggested that restoring the normal “good” bacteria, through consumption of yoghurt in these mice improved the leaky gut and reduced progression to kidney disease. Another study showed the immune system became more anti inflammatory when lupus-prone mice were given Lactobacillus found in probiotics, reducing kidney disease. There have been no published studies in human lupus so far.
Omega 3 fatty acids are essential polyunsaturated fatty acids which are vital dietary components as they cannot be made by humans. Three types exist, one found in plants and their oils such as walnut, pecans, flaxseed and hemp and the other two found in marine oils from fish including salmon, mackerel, sardines and anchovies.
Studies in populations e.g. Greenland Inuit, suggest a diet rich in oily fish may promote a reduced risk of cardiovascular disease. Animal studies also suggest omega 3 supplementation with calorie restriction may prolong lifespan. There is conflicting evidence for the use of omega 3 in lupus. Some studies support its benefits, but perhaps more robustly designed studies have failed to find any benefit in short term use (12 weeks) in indirect measures of cardiovascular disease, lipid profiles or lupus disease activity. The conflicting data may represent varying effects in the different populations studied, the use of different ways to measure lupus activity together with the problems of interpreting indirect measures of cardiovascular risk.
As lupus patients exhibit a higher risk of cardiovascular disease including heart
disease, these studies may be highly relevant. However, analysis of studies does not strongly support the use of omega 3 supplementation in practice. There is concern about whether omega 3 may increase the risk of prostate cancer and it is not certain whether it can be used by people who are allergic to shellfish or seafood.
Trace Elements
Magnesium is an important co-factor in multiple processes in the body including DNA and protein synthesis and enzymatic processes, including energy production. It is readily available in the diet of most people being abundant in nuts and green leafy vegetables. Most magnesium is inside cells so measurement in blood is not always a reliable guide to deficiency. Magnesium supplements have not been tested in lupus but have been tested in conditions which are relevant. A higher magnesium intake may reduce the risk of hypertension, heart disease and strokes. Magnesium is a standard therapy for the treatment of acute asthma attacks. Magnesium supplementa-tion inosteoporosis may improve bone turnover and improve bone density. In epidemiological studies, people with lower bone density tend to have lower blood magnesium levels reflecting the impact of magnesium of hormone important to bone turnover. Its most useful role in lupus may be in the treatment of migraine headaches which affects many people with lupus. Patients with migraine often have lower magnesium levels. When Magnesium is taken up to 600mg daily it may reduce migraine frequency and is classified by the American Academy of Neurologists as being of “probable” benefit. As this dose is far higher than the recommended daily dose, magnesium supplements should be discussed with the GP or lupus specialist. Side effects can include diarrhoea, flushing and low blood pressure and very high doses (very rare) can be fatal. Currently, no studies exist in lupus associated headaches or migraines and so its effectiveness in this setting is unknown.
Zinc is vital for many enzyme reactions, protein and DNA synthesis. The recommended daily intake, 11 mg in men and 8 mg in women, is important as it cannot be easily stored in the body. It is found in highest quantities in red meat, poultry and oysters but less so in vegetarian diets. Deficiency is most often caused by dietary insufficiency but also alcoholism and gastrointestinal diseases causing malabsorption including acute and chronic diarrhoea. Supplements of Zinc contain different forms and calculation may be required to determine if the quantities are sufficient.
Zinc deficiency can cause a compromised immune system with reductions in cell function and protection. Supplemental Zinc may have benefit when taken early for the common cold and could delay the onset of age-related macular degeneration but evidence in other conditions, particularly lupus, is currently lacking. Therefore, supplementation cannot be routinely recommended in lupus.
Selenium is stored in skeletal muscle and is incorporated into Selenoproteins, important in DNA synthesis and thyroid function. Meat and cereals contain selenium, the highest concentration is found in Brazil nuts. Selenium levels in blood can be low due to dietary insufficiency (not common in the western world), chronic gastrointestinal diseases and kidney dialysis patients.
There is limited evidence that selenium supplementation may reduce the incidence of some gastroin-testinal cancers but not others such as prostate cancer. Selenium in combination with Vitamin A, C and E was found to potentially reduce cognitive decline in one French study, but the independent effect of selenium was not clear. Lupus animal studies suggest selenium supplementation may improve immune function in some cells, while improving survival but with no overall effect on antibody production. Human lupus studies have not yet been conducted.
Defined Diets
Gluten is a storage protein component of cereals including wheat, barley, rye and oats. In genetically susceptible people, it can trigger immune mediated damage to the small bowel (coeliac disease, CD) causing malabsorption. The treatment of CD is a gluten-free diet, now widely available which has been used by patients with no known CD to improve their symptoms. There may be a link between lupus and CD and the two are found together more commonly than might be expected by chance.However, evidence supporting gluten free diets in conditions other than CD is sparse. No known scientific trials of gluten-free diets in lupus have been reported. Anecdotally, some lupus patients feel their bloating and abdominal pain may improve with a gluten-free diet, but it is important to ensure a healthy balanced diet is maintained to avoid missing other vital components of a good diet.
Paleo
The Paleo diet requires eating only those foods which were available to Palaeolithic humans with the premise being these diets are what humans evolved with and are superior to current diets. The calorific content of the Paleo diet should be 55% lean meat or fish, 15% vegetable, nuts, fruits with no sugar, added salt or dairy products. While there are some similarities between the Paleo diet and conventional diets e.g. Mediterranean diet, Paleo diets can lead to nutritional deficiency such as low calcium. There is no scientific evidence for using Paleo diets in lupus and, if used, must be with dietitian advice in conjunction with a lupus specialist.
FODMAPs (an acronym of Fermentable, Oligo, Di, Mono saccharides And Polyols are short chain carbohydrates poorly absorbed in the small intestine. They include lactose, fructose, sorbitol and mannitol, found in wheat, barley, rye, beans and pulses and fruits such as apples and avocados. FODMAP exclusion diets have been used with some evidence in the control of gastrointestinal symptoms in Irritable Bowel Syndrome (IBS). It is thought that
FODMAP’s attract water into the bowel and are easily fermented by bowel bacteria, generating methane and carbon dioxide gas. This expands the gut, stretching the nerves and causing abdominal pain. Fruits including melon and oranges, vegetables including carrot, chives and lettuce and breads and cereals such a quinoa and rice and gluten free bread are approved in low FODMAP diets.
While there are lupus patients who have IBS and could benefit from FODMAP exclusion, studies have not yet been done. Abdominal pain in lupus is often due to disease activity, with inflammation in the abdomen lining and bowel (serositis and vasculitis), so diets must be used with caution in conjunction with a lupus specialist rather than as an alternative therapy to replace lupus medications.
Alternative Medical Systems (Traditional Medicine)
Traditional medicine defines a group of interventions associated with historical practice including Ayurvedic and Traditional Chinese Medicines (TCM), the latter of which are covered by the National Health Insurance programmes in countries such as Taiwan.
Of 23084 newly diagnosed SLE patients in Taiwan between 1999 and 2009, 40% used traditional Chinese medicines for SLE treatment. This group had 27% lower risk of death compared to those who did not use these traditional medications. The TCM used included Zhi Bo Di Huang Wan (Rhizoma Rehmanniae, Fructus Corni, Poria Cocos amongst other ingredients) and Jia Wei Xaio Yao San (ingredients including Angelica sinensis, Atractylodes macrocephala). The reasons for the results are unclear, particularly as there is no clear mechanism for the action of these CAM treatments.
Another pilot study with 84 lupus patients in Hong Kong suggested that the Chinese herbal medication Zi Shen Qing (ZSQ) was associated with reduced disease activity measured by SLEDAI, reduction in steroid dose and reduced flare frequency. ZSQ consists of six herbs including radix astragali (Milk Vetch), Paeonia lactiflora (dry root of the peony) and the fruit of the dogwood Fructus Cornus.
Ayurvedic medicine is one of the world’s oldest medical systems. Its concepts of interconnectedness, the body’s constitution and life force (dosha) are individually determined and practitioners prescribe herbal remedies, lifestyle changes, exercises and diets. One study of 15 lupus patients using Ayurvedic medicine suggested improvement with relief of symptoms in 60% of patients. However, studies in lupus are limited in number and of low quality. In addition, 21% of 193 Ayurvedic products purchased over the Internet and manufactured in the USA or India contained unacceptably high levels of lead, mercury, and/or arsenic in one study. Other studies suggest Ayurvedic medicine can be superior to some conventional medicines such as methotrexate in Rheumatoid Arthritis, but care is needed to ensure Ayurvedic products are used with the aid of an experienced practitioner.
Mind-Body Interventions
Mind and body practices include diverse procedures or techniques administered or taught by a trained practitioner or teacher. The most popular mind-body interventions include yoga, chiropractic and osteopathic manipulation, meditation, and massage therapy. Acupuncture is discussed in another chapter.Yoga is an ancient Indian practice with the aim of uniting mind, body and spirit. The word is derived from the Sanskrit meaning “Union”. A systematic search of studies looking at musculoskeletal aspects of Yoga suggested a majority had small sample sizes while the largest with 100 patients had quality issues. However, Yoga was associat-ed with a trend to improvement in joint tenderness, pain, mood, increased energy and self-efficacy.
Yoga can be associated with improvements in gait, balance and flexibility but is likely to expend too little energy to benefit cardiovascular risk.
Few studies exist in lupus, but one in the USA recruited 57 lupus patients randomly assigned to Yoga or standard care. Patients were given 60-minute classes twice weekly for 8 weeks including gentle poses and home practice. A survey of the participants one week after finishing the programme indicated improvement in wellbeing, stress, pain management and sleep patterns. The improvements took some weeks to take effect with patients reporting feeling better well into the programme.
Tai Che and Qi Gong
Originally conceived as a martial art, Tai Chi is a centuries-old philosophy of Yin and Yang practiced through postures and movements with breathing, relaxation and mental focus being key. Qi Gong is a holistic series of breathing exercises, slow body movements and meditation, practiced for over 5000 years. There is some evidence that Tai Chi has benefit in Parkinson’s Disease, reducing pain in Osteoarthritis of the knee as well as fibromyalgia and other forms of chronic pain.
A recent 2017 study of 12 SLE patients with low levels of physical activity and high-perceived stress were given 2 Tai Chi classes per week and DVD home exercises the other 5 days. Stress levels fell, but levels of inflammatory chemicals (cytokines) also fell suggesting that the intervention reduced inflammation. Larger studies are needed to confirm the results while the mechanisms are still not clear. The effect of Qi Gong is more difficult to assess as no large studies have been done in lupus. However, a synthesis of several studies suggested some pain improvement with fibromyalgia, rheumatoid arthritis and osteoarthritis with various forms of Qi Gong including Taoist, Chaoyi Fanhuan and Baduanjin. Varying exercise times were used from 16 1.5 hr sessions to 45 60 min home programmes. Cognitive Behavioural Therapy (CBT).
CBT is a type of talking psychotherapy in which negative patterns of thought about self and the world are challenged so unwanted behaviour patterns or mood disorders such as depression, are changed. CBT is based on the concept that thoughts, feelings, physical sensations and actions are interconnected, and that negative thoughts and feelings can trap people in a vicious cycle. It focuses on current issues rather than on historical ones.
CBT may be helpful in irritable bowel syndrome and Chronic Fatigue Syndrome. The best evidence for CBT shown in an analysis of several studies (meta-analysis) is in anxiety, pain disorders and stress. In lupus, CBT may improve mood and reduce anxiety compared to control interventions. However, it may not always improve lupus blood test markers or disease activity levels, although some studies do report such an effect. In one study of 45 patients, stress, anxiety and mood were improved with CBT but no effect on disease activity was noted. In another study, 92 SLE patients were assigned to either CBT and biofeedback (a technique to increase body awareness and relaxation) or control groups using supportive counselling or standard medical treatment alone. The CBT+biofeedback group exhibited greater reductions in pain and psychological function, maintained for over 9 months, compared with the other two groups. However, disease activity improved in all three groups.
Meditation is the act of resting the mind and attaining a state of consciousness different to a normal waking state. It comprises one or more of many acts, including thought, contemplation, reflection and concentration. pressure in those at risk. It may also reduce anxiety and stress and, possibly, pain using Mindfulness Based Stress Reduction (MBSR) programmes. One small study of 30 SLE patients with kidney disease found that Buddhist meditation, taught by an experienced practitioner and instructed for 60 minutes a month but practiced daily for 24 weeks can improve mental and physical function. While stress hormones such as metanephrines were measured, no significant difference was found in levels between meditation and non-meditation groups. Meditation has been studied in high blood pressure, anxiety and pain. The evidence suggests Transcendental Meditation may be helpful in reducing blood pressure in those at risk. It may also reduce anxiety and stress and, possibly, pain using Mindfulness Based Stress Reduction (MBSR) programmes. One small study of 30 SLE patients with kidney disease found that Buddhist meditation, taught by an experienced practitioner and instructed for 60 minutes a month but practiced daily for 24 weeks can improve mental and physical function. While stress hormones such as metanephrines were measured, no significant difference was found in levels between meditation and non-meditation groups.
Manipulative and Body-Based Methods
These CAM systems focus on the structures and systems of the body including the joints, soft tissues, blood vessels and lymphatics. The two main systems are described.Spinal Manipulation
These procedures are practiced by osteopaths and chiropractors. The aim is to apply a force or movement to a joint in order to relieve pain. The most common indication for spinal manipulation is the treatment of back pain. Evidence suggests that spinal manipulation when practiced by a licensed practitioner, is as effective as painkillers and probably more effective than placebo, although the overall effect is probably small. Side effects include soreness at the site of manipulation and rarely, cauda equine syndrome where the lower spinal nerves become trapped, something which may require an operation to correct. There has been one report of tearing of the Carotid artery lining (dissection) in a pregnant lupus patient undergoing chiropractor treatment, and other similar reports in pregnancy have suggested neck manipulation may be a cause of these problems, but these reports are rare.
While spinal manipulation is an option in the treatment of back pain, whether painkillers, exercise or spinal manipulation are utilised, in some studies, fewer than 20% of patients are pain free after 18 months.
Massage therapy can encompass many techniques but all use fingers, hands, elbows, arms or feet, to rub, press or manipulate soft tissues in various areas. No large controlled studies exist for lupus but a case report of one patient suggests Swedish massage may help lupus flares.
Energy therapies surmise that practitioners can channel healing energy into a patient and effect improvement in wellbeing and disease activity. Several methods exist including hands-on, hands-off and distant, where the patient and practitioner are in different locations. Many people consider Energy Therapies as pseudoscience claiming very little evidence of any benefit and some evidence of lack of benefit. The US-based National Center for Complementary and Integrative Health (NCCIH) distinguishes between two types of Energy Therapies. The first involves scientifically observable energy, "Veritable Energy Medicine" (magnet therapy, colorpuncture and light therapy) and the second which invokes physically undetectable or unverifiable “energies”, which it calls "Putative Energy Medicine" (spiritual healing, Qigong healing, Reiki and crystal healing amongst others). However, organisations which fund studies of these therapies have been criticised by prominent researchers in complementary medicine for wasting money on funding poor quality research in these areas.
As an example, Reiki is a complementary health approach in which the practitioner places their hands on or just above a person to facilitate their own healing response. There is very little evidence for the use of Reiki in clinical studies and none in lupus. Using good quality research, Reiki was used in the painful condition, Fibromyalgia and found to be ineffective. The lack of evidence means that, at present, Reiki cannot be recommended as a useful intervention in lupus. In addition, there have been reports of sham practitioners who may suggest benefits which are not based on evidence and charge for the privilege. Other therapies such as Aromatherapy and Reflexology also lack evidence for their use with claims of benefit not currently backed up by objective science.
CAM products to avoid in lupus
Alfalfa (Lucerne) is most commonly used as an animal feed. However, it is used in some cuisines and has claimed health benefits because it contains several Vitamins including C and B complex. The raw seeds of the alfalfa plant contain high levels of an amino acid, L-canavanine which can stimulate immune cells. There have been several case reports of lupus flares with alfalfa and the advice is to avoid alfalfa completely.Echinacea (Coneflower) is part of the Daisy family. It has been used to treat a variety of conditions particularly flu and colds. The idea is that Echinacea may promote a stronger immune system. However, an analysis of several studies found no good evidence of benefit.
While the effect of Echinacea in lupus has not been formally tested, there have been reported cases of other immune conditions which flared after patients took Echinacea. It would be prudent to avoid it, especially as Echinacea may induce immune cells to secrete proinflammatory cytokines that can influence lupus.
Tripterygium wilfordii (Thunder God Vine)
Thunder God Vine is a perennial grown in China and Taiwan and used for over 2000 years in the treatment of inflammation. Thunder God Vine used in one Rheumatoid Arthritis study, could perhaps be better than a traditional drug, Sulphasalazine. It has also been used in lupus, and it seems to reduce levels of cytokines associated with inflammation such as IL-2. No properly controlled large trials exist in lupus, but open trials of over 200 patients suggest benefit with lupus skin rash, fatigue, joint pains and kidney function all improving. It may also reduce steroid requirements in some patients.
However, numerous side effects have been reported, including decreased bone density (Osteoporosis), infertility and hair loss. If not extracted carefully, the plant is poisonous and has been reported to cause death and may damage the unborn foetus. It would, therefore, be wise to avoid despite its claimed benefits.
Other toxic herbal remedies Several herbs can potentially cause kidney damage. Amongst these are aristolochic acid (A1), which originates from the Chinese herb Aristolochic fangchi, cat’s claw (Uncaria tomentos) and CKLS (colon, kidney, liver, spleen). Some herbs contain heavy metals that may be toxic. One study of 28 commonly used plants used to produce herbal remedies found high quantities of lead and cadmium with the leaf containing higher levels than the stem, bark or roots with the lowest levels in seeds.
Conclusion: Integrative Medicine: the best of both worlds?
Perhaps unwittingly, integrative medicine, which is the practice of combining conventional and complementary approaches to healthcare, is practiced widely because so many patients take CAM as part of their therapy with or without their doctor’s knowledge.What is clearly needed in this setting is greater co-ordination between the two approaches but also a more robust critical approach to CAM. Much more scientific evidence of the type used currently in testing new drugs is required to provide better evidence for, or to refute the actions of, many CAM therapies. Robust examination of studies by some groups suggest some of the evidence for CAM therapies discussed are of poor quality with poorly designed studies, inadequate numbers of participants with incorrect conclusions drawn.
There is no doubt that the use of CAM is highly relevant to the management of lupus. Benefits, hazards and interactions have all been reported with CAM and it is essential that the approach to CAM must include patients and their specialists discussing options together to ensure the safest and most effective outcome.
Dr Arvind Kaul
Consultant Rheumatologist
St. George’s Hospital
Tooting
London SW17 0QT

 ©2024 LUPUS UK (Registered charity no. 1200671)
©2024 LUPUS UK (Registered charity no. 1200671)